Spokane Valley's Best Periodontist
As we age, we do not necessarily have to lose our teeth. We have a fair chance of maintaining our natural teeth for the rest of our lives if we maintain good oral hygiene and have regular professional cleanings and inspections. In addition to the teeth themselves, this also refers to the supporting bone and gum tissues that surround the teeth. These supporting tissues are at danger due to gum disease, a bacterial infection. Dentists are constantly on the lookout for early warning signs that patients could overlook because of this. If warning signs emerge, periodontal therapy may be suggested.
The aim of periodontal therapy, which can take a variety of forms, is always to restore unhealthy tissues to their initial level of health. In the most severe cases, tooth loss may occur as a result of gum disease (also known as periodontal disease), which can spread from the gums to the bone that supports the teeth. Scalings (deep cleanings), surgical restoration of harmed gum and bone tissue, and calculus (tartar) removal from below the gum line are all effective therapies.

Periodontal Therapy Procedures
Periodontal therapy includes both surgical and non-surgical techniques to restore health to the tissues that support the teeth (gums and bone) and prevent tooth loss. They include:
- Scaling and Root Planing. These deep-cleaning techniques are the best starting point to control gum disease. Plaque and calculus (tartar) are removed from beneath the gum tissues, using hand scalers and/or ultrasonic instruments.
- Gum Grafting. Sometimes it’s necessary to replace areas of lost gum tissue so that tooth roots are adequately protected. This can be accomplished by taking healthy gum tissue from one area of the mouth and moving it to where it is needed, or by using laboratory-processed donor tissue.
- Periodontal Plastic Surgery. When used to describe surgery, the word “plastic” refers to any reshaping procedure that creates a more pleasing appearance of the gum tissues.
- Crown Lengthening Surgery. This is a surgical procedure in which tooth structure that is covered by gum and bone tissue may need to be exposed either for cosmetic reasons (too make the teeth look longer and the smile less gummy) or to aid in securing a new dental crown.
- Dental Implants. Today’s preferred method of tooth replacement is a titanium dental implant, which is placed beneath the gum line and into the jawbone during a minor surgical procedure. The implant is then attached to a realistic-looking dental crown that is visible above the gum line and indistinguishable from a natural tooth.
Your Role in Periodontal Health
Effective daily brushing and flossing are essential to preventing periodontal disease, which is mostly brought on by dental plaque. On the other hand, scrubbing can actually make your gums recede. We can show suitable procedures for you if you have any questions.
Of course, a toothbrush and floss can’t reach every area of the mouth, which is why routine professional cleanings at the dentist are so important. During your routine dental exam, the early stages of gum disease might be identified before they become obvious to you.
Eating a nutritious diet low in sugar, and staying away from tobacco in all forms, will also increase your periodontal health — and your chances of keeping your teeth for life.
Spokane Valley's #1 Periodontist - Periodontal Therapy Near Me - Gum Disease Treatments in Spokane Valley, PA
 While you may think that some loss of teeth is inevitable with aging, it is actually possible for all of your teeth to last a lifetime. One of the ways you can achieve this goal is to avoid periodontal disease (“peri” – around; “odont” – tooth), which is caused by bacteria that attack the tissues around the teeth. Unfortunately, you may not even realize you have gum disease as the signs and symptoms are not always as apparent to you as they are to a dental professional.
While you may think that some loss of teeth is inevitable with aging, it is actually possible for all of your teeth to last a lifetime. One of the ways you can achieve this goal is to avoid periodontal disease (“peri” – around; “odont” – tooth), which is caused by bacteria that attack the tissues around the teeth. Unfortunately, you may not even realize you have gum disease as the signs and symptoms are not always as apparent to you as they are to a dental professional.
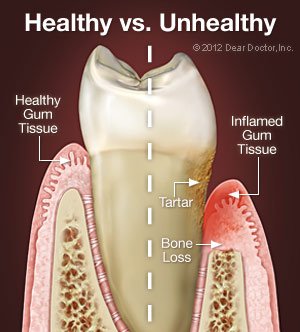
Nearly all people who do not maintain good daily oral hygiene will develop gingivitis. If left untreated, this bacterial gum infection can progress from gingivitis (“gingival” – gum; “itis” – inflammation) to periodontitis, which results in bone loss around your teeth. As the bone tissue is lost, the gum tissues detach from the teeth and form little pockets that provide an even better place for bacteria to live — where your brush and floss can’t reach. As periodontal disease advances leading to more bone loss, tooth loss can result. Part of this has to do with genetics, as periodontal disease tends to run in families. The good news is that periodontal disease can be controlled, even at more advanced stages.
Signs and Symptoms of Periodontal Disease
It’s important to understand that you can have periodontal disease with no obvious symptoms, especially if you are a smoker (nicotine reduces blood supply preventing bleeding and swelling of the gum tissues). Still, there are some important things to look for:
- Bleeding gums — Some people think that when their gums bleed, it simply means they’re brushing too hard. While brushing too hard is bad for the gums, it should not cause bleeding. Any bleeding of the gums should be considered a warning sign of gum disease.
- Bad breath — It’s very easy for plaque to collect in the spaces between the teeth, creating the perfect living conditions for bacteria that produce odorous, sulfur-containing compounds, resulting in bad breath.
- Redness or swelling of the gums — Inflammation of the gums is usually the first visible sign of periodontal disease.
- Receding gums — If you notice that your teeth look longer than they used to, it may be that your gum tissue has receded (away from the enamel), exposing some of your tooth roots.
- Sensitivity — If there is gum recession, the exposed roots may become sensitive to hot or cold.
- Periodontal abscess — Bacteria can become enclosed in a periodontal pocket and the area will fill with pus, becoming swollen and painful.
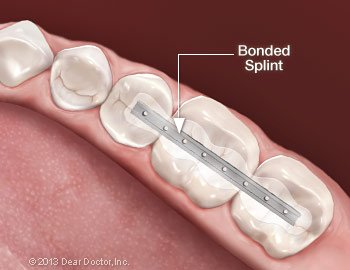
- Loose teeth — When periodontal disease results in bone loss, teeth can become loose or migrate. Tooth loss can result and may be accelerated if you are applying excessive biting forces from clenching or grinding your teeth.
Treatment Options in Spokane Valley
All periodontal therapy starts with the evaluation of your oral hygiene techniques and instruction for improving them, followed by the mechanical removal of plaque and any calcified deposits (tartar or calculus) that are present on the root surfaces. This is accomplished with a cleaning technique known as scaling, root planing or debridement using hand instruments and/or ultrasonic (high frequency vibrational) instruments. Locally applied antimicrobial products or antibiotics might also be recommended during various parts of periodontal treatment to assist in healing and pocket-depth reduction, hopefully eliminating the need for periodontal surgery. Sometimes surgical procedures may be necessary to remove the deep pockets that form between inflamed gum tissue and teeth. There are many different types of surgery to handle a variety of problems. And many times, combinations of procedures are used to attempt to reduce the number of surgeries as well as the cost of treatment.
Periodontal Disease & Your Overall Health
Periodontal disease starts in your mouth but has actually been linked to more serious conditions, such as cardio-vascular disease (CVD), diabetes and preterm births. Research has suggested two plausible mechanisms for how gum disease and these other serious medical concerns could be related: moderate to severe periodontal disease increases the level of systemic (bodily) inflammation — a characteristic of all chronic inflammatory diseases. Also, the same bacterial strains that are commonly found in periodontal pockets surrounding diseased teeth have been found in blood vessel plaques of individuals with CVD. Therefore, it may be helpful to reduce periodontal inflammation to reduce systemic inflammation.
Preventive Strategies
The best way to prevent periodontal disease is to brush and floss your teeth effectively every day. Regular dental checkups and professional cleanings every 3 or 4 or 6 months are also an important part of maintaining periodontal health; the instruments and techniques used in these cleanings can reach into areas that your toothbrush and floss can’t.
It is also possible to detect early forms of gum disease by evaluating your gingival (gum) tissues, both visually and by examining their attachment levels to the teeth. And the health of your tooth-supporting bone can be assessed by taking dental radiographs (x-rays pictures).
There are other steps you can take: Eating right, reducing stress in your life, and giving up unhealthy habits like smoking will also help ensure that you keep your teeth for a lifetime.
 After a thorough, professional tooth cleaning, you know that your teeth look brighter and feel fresher. But tooth cleaning isn’t just about appearances. It’s the primary means of preventing and treating periodontal (gum) disease. Many studies have demonstrated a possible link between periodontal health and overall (systemic) health — which means regular tooth cleaning may benefit not just your mouth, but your whole body.
After a thorough, professional tooth cleaning, you know that your teeth look brighter and feel fresher. But tooth cleaning isn’t just about appearances. It’s the primary means of preventing and treating periodontal (gum) disease. Many studies have demonstrated a possible link between periodontal health and overall (systemic) health — which means regular tooth cleaning may benefit not just your mouth, but your whole body.
Why do teeth need special cleaning? Over time, dental plaque (a naturally occurring bacterial biofilm) and stains build up on tooth surfaces. Dental calculus (also called tartar), a harder deposit, can then form both above and below the gum line. A thorough dental cleaning removes these substances from the teeth, and helps keep disease-causing bacteria from proliferating.
Tooth cleaning is usually accomplished by the non-surgical technique of scaling, sometimes called “root debridement.” It’s typically a relatively painless procedure in which small dental instruments are used to physically remove deposits from the surfaces of teeth. At one time, scaling was performed entirely with manual tools. But in the last several decades, the ultrasonic scaler has changed all that.
What Is An Ultrasonic Scaler?
There are different types of ultrasonic scalers, but all of them work in a similar fashion: electromagnetic forces in the unit’s hand-held “wand” cause its tiny tip to vibrate rapidly. These vibrations, which occur at a rate faster than the speed of sound, effectively blast away plaque, calculus and stains from the tooth surfaces.
A small stream of water and/or antibacterial mouthwash, which emerges near the tip of the scaler, is called lavage. Lavage is used to cool the ultrasonic scaler’s tip and flush away debris from the area being treated. The vibrating tip causes some of the water to break into millions of tiny bubbles, an effect called cavitation. This ruptures the walls of bacterial cells and helps create an environment that’s less hospitable to harmful bacteria.
Ultrasonic Scaling vs. Hand Scaling
Studies show that a thorough ultrasonic cleaning takes about one-third less time as compared to hand scaling — which means you need less time in the chair. Many patients prefer ultrasonics to other types of scaling, possibly because it requires the clinician to use less force than a hand scaler to get the same effect. In ultrasonic scaling, only the tip of the tool touches the tooth surface, and only for a short time.
It’s also possible to remove deposits of plaque and tartar from under the gum line by using an extremely small tip on an ultrasonic unit, which can cause less discomfort and result in a deeper and better cleaning. Sometimes an ultrasonic scaler is used first, and then any stubborn areas are scaled by hand.
The Experience of Ultrasonic Scaling
Anyone who has a substantial buildup of tartar or is prone to gum disease can benefit from ultrasonic scaling. It can also help to remove stains from coffee and cigarettes, for example. Yet, for all its power, most people experience little or no discomfort during the procedure.
If you have very sensitive teeth, it may be possible to alleviate some discomfort by using slimmer tips on the scaler. Alternatively, a topical anesthetic may be applied, or conscious sedation can be administered. The power range, the flow of lavage water and the frequency of tip vibration may also be adjusted for increased comfort.
Special tips are also available to clean composite or porcelain tooth restorations, titanium implants, or areas of demineralization (enamel loss) on your teeth. If you have a cardiac pacemaker, be sure to alert all dental professionals/personnel before ultrasonic scaling treatment, so precautions can be taken.
 When advanced gum disease (periodontitis) develops, your teeth are in danger: At this stage, the ligaments and bone tissue that surround them are being destroyed, and you could even begin losing teeth! If the disease can’t be controlled by non-surgical treatments like cleaning and scaling, then periodontal flap surgery may be your best treatment option.
When advanced gum disease (periodontitis) develops, your teeth are in danger: At this stage, the ligaments and bone tissue that surround them are being destroyed, and you could even begin losing teeth! If the disease can’t be controlled by non-surgical treatments like cleaning and scaling, then periodontal flap surgery may be your best treatment option.
Flap surgery is today’s leading method for treating and repairing periodontal pockets. What are these “pockets?” They are areas below the gum line where gum tissue has detached from the teeth, resulting in an uncleansable space where harmful bacteria can proliferate. These bacteria cause inflammation of the tissues, resulting in sensitivity, bleeding, and pain. Left untreated, they can cause a host of problems including gum disease, loss of the tooth-supporting bone structure, and possibly even systemic (whole-body) problems.
When periodontal pockets develop, the first step in treating them is usually via cleaning and scaling (also referred to as root debridement) with a manual or ultrasonic instrument. If this isn’t effective, then periodontal surgery is considered. Flap surgery isn’t a cure for periodontal disease — but it helps create an environment that makes it easier to maintain your periodontal health. And even if you’re prone to gum disease, proper professional treatment and regular care at home can help keep your teeth healthy for as long as possible.
The Goals of Flap Surgery
One major objective of flap surgery is to eliminate or reduce the pocket itself. To access it, a flap-like incision is made in the gum tissue. This allows diseased tissue to be removed from inside the pocket, and provides access to the teeth’s root surfaces for a thorough cleaning, which helps to eliminate harmful plaque and calculus (tartar). Afterward, the “flap” is closed, sealing the area. This begins the healing process, which takes place rapidly.
Another goal is the regeneration of periodontal ligament and bone tissue which may have been lost to the disease. A variety of techniques may be used to accomplish this, including high-tech methods of bone grafting and chemicals referred to as growth factors. These approaches help restore the gums to their normal form and function, and promote the healthy and secure anchoring of teeth.
The Flap Surgery Procedure
Flap surgery is typically done under local anesthesia, sometimes accompanied by oral anti-anxiety medications; alternatively, it may be performed under intravenous conscious sedation. After anesthesia has taken effect, a small incision is made to separate the gums from the teeth. The outer gum tissue is gently folded back to give access to the roots and the supporting ligament and bone tissue.
Next, the inflamed gum tissue can be removed, and the tooth roots can be cleaned; if needed, the area may also be treated with antibiotics or other medications. Bone defects can be repaired with grafting material, and proper regeneration of the periodontal ligament can be encouraged by physical (barrier membranes) and chemical (growth factors) methods. Finally, the incision is closed and the procedure is completed.
Performed by an experienced hand, state-of-the-art flap surgery has an excellent track record and offers well-established benefits. It’s often the treatment of choice for relieving periodontal disease and helping to maintain your oral health — and preserve your teeth.
 Maintaining good oral health has many rewards: A sparkling smile, fresh breath, and healthy gums. But recent scientific evidence suggests that it may have an even greater benefit to your overall health: Specifically, it could potentially reduce your risk for a number of systemic (whole-body) diseases, including cardiovascular disease (CVD), diabetes, and rheumatoid arthritis — even premature birth.
Maintaining good oral health has many rewards: A sparkling smile, fresh breath, and healthy gums. But recent scientific evidence suggests that it may have an even greater benefit to your overall health: Specifically, it could potentially reduce your risk for a number of systemic (whole-body) diseases, including cardiovascular disease (CVD), diabetes, and rheumatoid arthritis — even premature birth.
Periodontal (gum) disease is estimated to affect nearly half of all Americans, and is the major cause of adult tooth loss. Numerous studies have shown that patients with severe periodontal disease are at increased risk for developing cardiovascular disease. Periodontitis may also increase the chance that diabetes will develop or progress, and research suggests an association between gum disease and adverse pregnancy outcomes as well.
Inflammation: Friend and Foe
What’s the link between diseases of the mouth — like gum disease — and those of the body? They are connected by the body’s natural reaction to harmful stimuli, which we call the inflammatory response. Often characterized by pain, redness and swelling, inflammation is a process by which your immune system responds to damage or disease in your tissues. Inflammation can help the body heal — or, if it becomes chronic, it can lead to more serious problems.
Gum disease (periodontitis), CVD, diabetes and rheumatoid arthritis are all associated with the same type of inflammatory response. Studies have found that moderate to severe periodontitis tends to increase the level of systemic inflammation — a condition that may smolder in the background, awaiting the right conditions to flare into a more serious disease. It has also been shown that the same strains of bacteria that are found in inflamed gum tissue may also appear in the arterial plaques of individuals suffering from CVD.
How Does It Work?
While there is intriguing evidence of a link between gum disease and other systemic diseases, further studies will be needed to prove whether one causes the other. At present, however, several mechanisms have been proposed to explain how the connection works. One suggestion is that oral bacteria themselves may enter the bloodstream, form into clumps, and trigger systemic inflammation. The inflammatory response can cause swelling of cells and tissues, which narrow the arteries and increase the risk of blood clots.
Another possibility is that byproducts of oral bacteria released into the bloodstream could trigger the production of substances called CRPs (C-reactive proteins) in the liver. These proteins tend to inflame blood vessels and promote the formation of clots, possibly leading to clogged arteries, heart disease and stroke. Elevated CRP levels, according to some studies, are a stronger predictor of heart attack than cholesterol levels.
What You Can Do
Since chronic inflammation is a systemic problem, the best way to begin controlling it is via a whole-body approach. Maintaining a healthy weight, getting moderate exercise (and, if you use tobacco, quitting the habit) will help with this. So will bringing untreated inflammatory diseases, such as periodontitis, under control.
There are a number of effective treatments for periodontal disease, including nonsurgical procedures such as root cleaning and the local application of antimicrobials. For more serious conditions, conventional or laser gum surgery is an option. Finally, to keep your gums healthy between office visits, you need to develop an effective oral hygiene routine you can practice at home.
Although it’s too early to say that periodontal disease causes heart disease or other systemic conditions, they seem to have a connection. And while medicine and dentistry can’t change genetics, together we can control external factors like excess weight, tobacco use… and gum disease. Maintaining good oral hygiene is the best way to avoid periodontal problems. But if problems occur, don’t wait: The sooner you have treatment, the better your chances for controlling gum disease — and perhaps systemic diseases too.
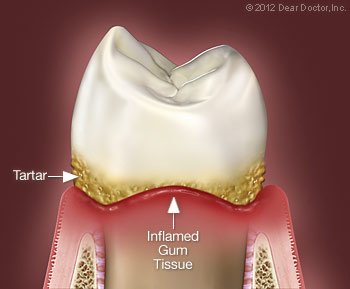 Periodontal (gum) disease is an infection caused by bacterial plaque, a thin, sticky layer of microorganisms (called a biofilm) that collects at the gum line in the absence of effective daily oral hygiene. Left for long periods of time, plaque will cause inflammation that can gradually separate the gums from the teeth — forming little spaces that are referred to as “periodontal pockets.” The pockets offer a sheltered environment for the disease-causing (pathogenic) bacteria to reproduce. If the infection remains untreated, it can spread from the gum tissues into the bone that supports the teeth. Should this happen, your teeth may loosen and eventually be lost.
Periodontal (gum) disease is an infection caused by bacterial plaque, a thin, sticky layer of microorganisms (called a biofilm) that collects at the gum line in the absence of effective daily oral hygiene. Left for long periods of time, plaque will cause inflammation that can gradually separate the gums from the teeth — forming little spaces that are referred to as “periodontal pockets.” The pockets offer a sheltered environment for the disease-causing (pathogenic) bacteria to reproduce. If the infection remains untreated, it can spread from the gum tissues into the bone that supports the teeth. Should this happen, your teeth may loosen and eventually be lost.
When treating gum disease, it is often best to begin with a non-surgical approach consisting of one or more of the following:
- Scaling and Root Planing. An important goal in the treatment of gum disease is to rid the teeth and gums of pathogenic bacteria and the toxins they produce, which may become incorporated into the root surface of the teeth. This is done with a deep-cleaning procedure called scaling and root planing (or root debridement). Scaling involves removing plaque and hard deposits (calculus or tartar) from the surface of the teeth, both above and below the gum line. Root planing is the smoothing of the tooth-root surfaces, making them more difficult for bacteria to adhere to.
- Antibiotics/Antimicrobials. As gum disease progresses, periodontal pockets and bone loss can result in the formation of tiny, hard to reach areas that are difficult to clean with handheld instruments. Sometimes it’s best to try to disinfect these relatively inaccessible places with a prescription antimicrobial rinse (usually containing chlorhexidine), or even a topical antibiotic (such as tetracycline or doxycyline) applied directly to the affected areas. These are used only on a short-term basis, because it isn’t desirable to suppress beneficial types of oral bacteria.
- Bite Adjustment. If some of your teeth are loose, they may need to be protected from the stresses of biting and chewing — particularly if you have teeth-grinding or clenching habits. For example, it is possible to carefully reshape minute amounts of tooth surface enamel to change the way upper and lower teeth contact each other, thus lessening the force and reducing their mobility. It’s also possible to join your teeth together with a small metal or plastic brace so that they can support each other, and/or to provide you with a bite guard to wear when you are most likely to grind or clench you teeth.
- Oral Hygiene. Since dental plaque is the main cause of periodontal disease, it’s essential to remove it on a daily basis. That means you will play a large role in keeping your mouth disease-free. You will be instructed in the most effective brushing and flossing techniques, and given recommendations for products that you should use at home. Then you’ll be encouraged to keep up the routine daily. Becoming an active participant in your own care is the best way to ensure your periodontal treatment succeeds. And while you’re focusing on your oral health, remember that giving up smoking helps not just your mouth, but your whole body.
Often, nonsurgical treatment is enough to control a periodontal infection, restore oral tissues to good health, and tighten loose teeth. At that point, keeping up your oral hygiene routine at home and having regular checkups and cleanings at the dental office will give you the best chance to remain disease-free.
 Even if you brush and floss your teeth faithfully, it is important that you have your teeth professionally cleaned on a regular basis. (Of course, if you aren’t quite so meticulous about your oral hygiene, it’s even more important!) After a thorough cleaning, your teeth will feel smooth and squeaky-clean, and they will probably look a lot brighter too. But professional teeth cleanings aren’t done for looks alone.
Even if you brush and floss your teeth faithfully, it is important that you have your teeth professionally cleaned on a regular basis. (Of course, if you aren’t quite so meticulous about your oral hygiene, it’s even more important!) After a thorough cleaning, your teeth will feel smooth and squeaky-clean, and they will probably look a lot brighter too. But professional teeth cleanings aren’t done for looks alone.
Why do your teeth need this kind of attention? Essentially, it’s because over time they tend to build up a layer of plaque (a sticky, bacteria-rich film) and hard deposits (called tartar, or calculus) that are very difficult to remove without special tools. When these deposits are allowed to remain on the tooth surfaces or below the gum line, they provide ideal conditions for bacteria to grow and multiply. The acids produced by some bacteria cause tooth decay and gum disease; if left uncontrolled, this can lead to inflammation and infection of the gums, and possibly influence systemic (whole body) diseases.
Dentists have a special term for preventive procedures like tooth cleaning: prophylaxis, from the Greek word meaning to protect or guard against. In this case, the focus is on preventing tooth decay and gum disease. Performed in conjunction with a routine dental examination, a professional cleaning can go a long way toward controlling these two common maladies. While your teeth are being cleaned, it’s also a good opportunity to take a close look at your oral health in general and check for a few specific problems.
The Professional Cleaning Procedure
Teeth cleaning is often performed by a dental hygienist — a highly trained technician who uses a special set of tools designed just for this purpose. Because everyone’s teeth are a little different, your cleaning will be tailored to your particular needs. However, many cleanings follow a similar pattern.
First, the dental hygienist will do an oral examination to evaluate the health of your oral tissues. Then the cleaning will take place using either an ultrasonic scaler or metal instruments referred to as curettes to remove the plaque and calculus from the tooth surfaces. The ultrasonic scaler is a hand-held tool with a tiny tip that vibrates at a very high frequency. Hardened deposits are broken up by the rapid movement of the tip, which does not damage the tooth. A constant stream of liquid (called lavage) serves to cool the tip and aid in plaque removal; at the same time, it also washes away the debris.
Some hygienists prefer curettes, which are hand-held instruments that are curved and tapered to fit around and in between the teeth. If your teeth are sensitive, using hand-held instruments may be more comfortable for a professional cleaning. In the capable hands of a hygienist or dentist, it takes only moderate pressure to remove any stubborn buildup and scrub the teeth clean, regardless of which instruments are used.
Finally, your teeth are polished with a low-speed rotary brush fitted with a soft rubber tip. A slightly gritty, toothpaste-like gel is applied, and the tip spins around and polishes the teeth, making them smooth and shiny.
A Requirement for Good Oral Health
Most people don’t feel any noticeable discomfort during dental cleanings; some even report they enjoy the experience — especially the dramatic results when it’s done! If you haven’t had a cleaning in a while, however, it may take you a few moments to get used to getting your teeth cleaned. If you experience any discomfort, however, it may be possible to apply a topical numbing gel or another type of anesthetic.
If your gums are irritated due to bacterial buildup, they may become sore or bleed slightly during the cleaning. It may be possible to prevent this from occuring in the future with oral hygiene measures you can perform at home (such as improved flossing techniques or special mouthrinses); it might also indicate that you need more frequent in-office cleanings. This type of regular maintenance will help you avoid more involved dental procedures down the road — and it will give you the best chance of keeping your teeth for life!
 If gum recession is affecting your health or your appearance, a procedure called gingival (gum) grafting may be recommended. Although it might sound scary, a variety of gum grafting procedures are routinely performed by periodontists (specialists in the area of gingival tissue), and by some general dentists with specialized training in this field.
If gum recession is affecting your health or your appearance, a procedure called gingival (gum) grafting may be recommended. Although it might sound scary, a variety of gum grafting procedures are routinely performed by periodontists (specialists in the area of gingival tissue), and by some general dentists with specialized training in this field.
Gum grafting involves carefully placing a small amount of new tissue in an area where little or no gum tissue currently exists — typically recommended to prevent further gum recession or to cover root surfaces of your teeth that have become exposed. The tissue used in this procedure may come from a variety of sources but usually is taken from the palate (roof of the mouth), after the area has been numbed for your comfort. Then it is delicately sutured (stitched) in place where it’s needed, using suturing material which may be finer than a human hair.
Your body’s natural recovery process takes over after the grafting procedure is complete. During this time, new blood vessels grow into the graft and help it to become integrated with the surrounding tissue. A successful graft can reduce or eliminate problems like tooth sensitivity and further gum recession, as well as improve the aesthetics of your smile.
How do you know if you need a gum graft? Often, you can clearly see or feel the problem. Exposed tooth roots can make your teeth look overly “long,” and they also generally appear somewhat darker than your pearly white crowns. Gum recession is a condition that can increase with age, as we recognize when we hear the phrase “long in the tooth.” But the potential problems of gum recession aren’t just cosmetic — they can also seriously impact your oral health.
A Closer Look at Your Gums
Inside your mouth, gum tissue forms a barrier that resists the vigorous mechanical (and microbial) effects of eating, chewing and biting. Gums may begin to recede, or shrink down, for several reasons.
One is ineffective oral hygiene: This includes both inadequate brushing, which fails to remove dental plaque; and excessive brushing, which erodes the tissue. Foreign objects in the mouth that rub against the gums, like poorly fitting removable dentures, tongue bolts, or even fingernails, can also contribute to gum recession.
When the tooth’s roots lose the protection of healthy gum tissue, they can become extremely sensitive to hot or cold temperatures, causing pain when you consume many foods and drinks. Worse, missing gum tissue makes it easier for bacteria to penetrate the roots and cause decay — or for minor trauma to result in rapid gum recession. In either case, the eventual result may be tooth loss. That’s why proper treatment of gum recession is so important.
Treating Gum Recession With Gingival Grafting
After a thorough examination and assessment of your teeth, gums and overall health, the gingival grafting procedure may be recommended. The tissue used in this procedure may be obtained from a variety of sources: an area next to the area of recession, from the hard palate, or donated tissue from another person, which has been medically processed to make it safe to use.
There are several different methods of grafting. For example, if you have lost gum tissue in an area of your mouth that’s not highly visible when you talk or smile, additional gum tissue can be placed there to prevent further recession without trying to cover the tooth-root surface completely. This procedure is referred to as a free gingival graft (since the tissue is separated from its blood supply), and it takes about 45 minutes to perform. It is very predictable with a very high success rate. If the objective is to cover root surfaces, the procedure becomes more complicated and will take longer, but is still very successful.
Grafting procedures are typically carried out under local anesthesia, and are generally pain-free. You should experience very little discomfort after the surgery, even if tissue has been removed from your palate, because that donor area is usually covered by a soothing, liquid band-aid-like material. Fortunately, any discomfort that you do have can be alleviated with over-the-counter or prescription anti-inflammatory medication, and it is generally short-lived. A soft diet (and an antibiotic) may also be recommended for a week or so thereafter, enabling the tissues to heal fully; otherwise, your normal activities will not be limited.
Keeping Your Gums Healthy
Following a gum graft, it’s more important than ever to practice good oral hygiene; this will help prevent gum problems from developing in the future. Your regimen should include proper brushing with fluoride toothpaste, daily flossing, a healthy diet and regular dental and periodontal checkups. Maintaining healthy gums is a key to keeping up your overall oral health — and preserving your smile.
 There are many elements that make up an ideal smile; bright, healthy-looking teeth immediately come to mind. But the gum tissue that surrounds and supports those teeth also plays a big role in how appealing your smile will look.
There are many elements that make up an ideal smile; bright, healthy-looking teeth immediately come to mind. But the gum tissue that surrounds and supports those teeth also plays a big role in how appealing your smile will look.
There are various cosmetic issues involving gum (gingival) tissue. For example, your smile may look “gummy” — meaning you seem to display too much gum tissue when you smile, or your teeth appear too short. Sometimes it’s the opposite problem — your teeth appear too long because your gum tissue has receded (pulled back), exposing tooth-root surfaces that were covered at one time. Or, you may have an uneven gum line, meaning gum tissue covers some of your teeth more than others. All of these cosmetic gum problems can be successfully treated with cosmetic procedures performed in the dental office.
Cosmetic Gum Problems
Excess Tissue. A gummy smile can be caused by excessive gum tissue covering more enamel surface of a tooth’s crown (upper portion) than normal. If that is the case, a procedure known as “crown lengthening” can be performed, in which gum tissue (and sometimes a small amount of bone tissue) is removed to expose more tooth surface.
Receding Gums. Sometimes your gums can shrink down (recede), exposing a portion of your tooth roots. This causes a cosmetic problem because root surfaces, which have no enamel covering, tend to appear more yellow than the crowns of your teeth. Also, exposed roots can be more sensitive to cold or touch, and can be at greater risk of decay. There are various gum-grafting procedures that can cover exposed roots, all of which involve moving gingival (gum) tissue from one site in the mouth to another. For example, roots can be covered with tissue from the roof of your mouth, which is of the same type; or adjacent (nearby) tissue can be moved over to cover an exposed root. Sometimes laboratory-processed tissue from another donor can even be used. All of these options can be discussed with you in more detail.
Uneven Gum Line. If you have an uneven gum line where some teeth are covered by more tissue than others, it is often possible to recontour (reshape) the tissue for a very pleasing effect. This can be done conventionally with a surgical scalpel or with newer dental laser technology. The advantage of a laser is that it seals the tissue as it sculpts it, making the procedure more comfortable and requiring a shorter healing time.
What to Expect From Gum Grafting
All cosmetic gum surgery can be performed at the dental office — and it usually requires only a local anesthetic (numbing shot). In fact, for laser surgery you may need only a topical anesthetic applied in gel form. If you would like a deeper level of relaxation, you can have oral or possibly even an IV sedative; but if this is required, you will need a ride home. Laser surgery leaves no open wounds and causes minimal, if any, discomfort, though the anatomy of the area may preclude laser use. An examination is required to determine whether conventional or laser treatment is in your best interests.
Grafts may take longer to heal, particularly if tissue is taken from the roof of your mouth. If that’s the case, you will have two sites that need to heal: the donor site from which the tissue was taken, and the recipient site where the tissue was attached. Both of these sites will require stitches, usually of the dissolving type. You will need to eat a softer diet and avoid chewing on that side of your mouth for a few days. Though full healing may take a few weeks, you will be able to resume your normal activities the very next day. Whichever kind of cosmetic gum surgery you may need, the procedures are routine and predictable — and they can do wonders for your smile!
 When you are a child, your first loose tooth can be cause for celebration; when you are an adult, it definitely is not. Biting and chewing with a tooth that is not securely attached in its socket can be difficult or even painful — and any tooth that becomes loose is at risk of needing to be removed or, at worst, falling out. It’s often possible to prevent that from happening, but quick action is required.
When you are a child, your first loose tooth can be cause for celebration; when you are an adult, it definitely is not. Biting and chewing with a tooth that is not securely attached in its socket can be difficult or even painful — and any tooth that becomes loose is at risk of needing to be removed or, at worst, falling out. It’s often possible to prevent that from happening, but quick action is required.
Causes of Loose Teeth
The most common reason for tooth looseness is periodontal disease — a bacterial infection of the gum and/or bone tissues that surround and support your teeth. The infection results from bacterial plaque that sits on your teeth in the absence of effective oral hygiene. Over time, periodontal disease will cause gum tissue to detach from the teeth as plaque and tartar formation increases and tooth-supporting bone is lost. As more bone is lost, teeth gradually become loose and are unable to withstand normal biting forces. If severe periodontal disease remains untreated, loose teeth will eventually fall out.
Another common contributor to the loosening of teeth is a clenching or grinding habit that generates too much biting force. This force can stretch the periodontal ligaments that join the teeth to the supporting bone, making your teeth looser. These habits can accelerate bone loss and also cause jaw pain and excessive tooth wear.
Treatment for Loose Teeth & Bite Issues
Just as the causes of loose teeth can be biological (disease) or mechanical (too much force) — or both — so, too, are the treatments. Let’s first take a look at the biological approach.
To control gum disease, a dental professional must thoroughly clean the teeth of plaque and harder deposits (tartar or calculus) in which bacteria thrive; this includes the tooth-root surfaces beneath the gum line. At the same visit, you will be instructed on effective oral hygiene techniques and products to use at home. Often this type of deep cleaning, combined with improved oral hygiene, will reduce inflammation and heal the gums enough to cause some tightening of the teeth.
The mechanical approach involves modifying the forces that are applied to the teeth. This can be achieved in a number of ways. For example, an occlusal (bite) adjustment can be performed by carefully reshaping minute amounts of tooth surface enamel. This changes the way upper and lower teeth contact each other, redirecting and lessening the force. Replacing broken fillings and restoring worn teeth is also sometimes needed to create a more balanced bite, even when teeth are not loose.
It is also possible to reduce stresses on teeth by temporarily or permanently splinting them together like fence pickets so that any biting force is distributed among groups of teeth rather than individual loosened teeth. The splint is a very small metal bracket bonded to the backs of or tops of the teeth.
If clenching or grinding habits are a problem, a custom-made bite guard (also called an occlusal splint) can be worn when needed. Placed in the mouth at night or in times of stress, it can protect the teeth from the consequences of too much biting force. This can also be helpful in preventing excessive tooth wear, and sometimes in relieving jaw pain.
Loose teeth can be successfully treated with both biological and mechanical techniques. A thorough examination will be needed to determine the best approach. So if you are experiencing tooth looseness, don’t wait — the sooner this problem is addressed, the more likely you are to keep your natural teeth.
Meet Your Top-Rated Family Dentist in Spokane Valley

Our Dental Services
Dental Crowns
Emergency Care
General Dentistry
Implant Dentistry
Orthodontics
Pediatric Dentistry
The Proof is in our Patients