Spokane Valley's Best Pediatric Dentist
Your child’s first teeth aren’t going to last forever, but that doesn’t mean they don’t require special attention. Primary (baby) teeth serve several incredibly vital tasks, thus maintaining your child’s oral health early will bring health benefits far into adulthood.
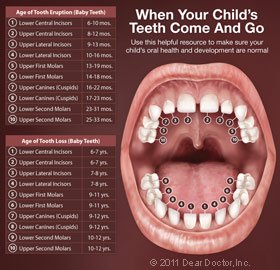
Primary teeth, for example, function as guides for the eruption of permanent (adult) teeth, holding the area in which these new teeth would erupt. The permanent teeth’s crowns (tops) press against the roots of the baby teeth, causing them to resorb (melt away). Adult teeth can then be placed in their right positions.
Furthermore, your child’s primary teeth will be present for the most of his or her childhood, assisting your youngster with biting, chewing, and speaking. For the first six years or so, he or she will rely solely on primary teeth to fulfill these vital duties. Your youngster will have a mixture of primary and permanent teeth until about the age of 12. You’ll want to keep those teeth healthy and lose them naturally when the time comes.

Treatment of Your Child's First Teeth
Your child’s 20 baby teeth will arrive between the ages of six and nine months, though it could happen as early as three months or as late as twelve months. The lower front teeth emerge first, followed by the higher front teeth. The canines appear next, followed by the first molars (eyeteeth). During this process, your baby may feel teething discomfort. If this is the case, there are steps you may take to assist your youngster feel more at ease.
After each feeding, gently wipe your infant’s gums and newly erupted teeth with a water-soaked gauze pad or damp washcloth. Establish a daily brushing habit using a small, soft-bristled toothbrush and no more than a thin smear of fluoridated toothpaste starting at age 2, when there are more teeth in the mouth. Your youngster may require your assistance with this vital chore until he or she reaches the age of six.
Your Child's First Dental Appointment
The American Academy of Pediatric Dentistry recommends that your child see a dentist by his/her first birthday. Though this may sound early, learning proper pediatric oral hygiene techniques, checking for cavities, and watching for developmental problems is extremely important.
There are a number of forms of tooth decay that can affect babies and small children. Early Childhood Caries (tooth decay) can develop rapidly, progressing from the hard, outer enamel layer of a tooth into the softer, inner dentin in six months or less.
Most of all, it’s important for your child to have a positive experience at the dental office as he/she will be a regular visitor for years to come.
Pediatric Dental Treatments
There are a variety of dental treatments offered to prevent tooth decay in children, or to save or repair teeth when necessary. They include:
Topical Fluoride — Fluoride incorporates into the enamel of teeth, making it harder and more resistant to decay. Although there is a small amount of fluoride in toothpastes and in some drinking water supplies, a higher concentration can be applied professionally to your child’s teeth for maximum protection.
Dental Sealants — A plastic coating can be applied at the dental office to prevent cavities by sealing the little grooves on the chewing surfaces of back teeth known as “pits and fissures.” These little crevices become the perfect environments for decay-causing bacteria. Immature tooth enamel is more permeable and therefore less resistant to tooth decay. Dental sealants are easy to apply and provide years of protection.
Root Canal Treatment — Perhaps you have had a root canal treatment yourself, to save an injured or severely decayed tooth. Well, sometimes children need root canals, too. As mentioned above, baby teeth are important guides to the permanent teeth that are already forming beneath your child’s gums. Therefore, saving them from premature loss can help prevent a malocclusion (“mal” – bad; “occlusion” – bite) that requires orthodontic treatment.
Bonding — Chips and minor fractures to front teeth — common childhood occurrences — can be repaired with tooth-colored bonding materials. These lifelike resins made of plastic and glass can be used on baby teeth as well as permanent teeth and last until the youngster has completed facial growth.
Your Child & Orthodontics
Most malocclusions are visible by the age of seven. Interceptive orthodontic treatment at this age can help direct optimal tooth alignment and/or jaw growth, reducing or eliminating the need for later orthodontic treatment. Many orthodontic problems can be recognized early, which is why your child should be evaluated by a skilled specialist during his or her growth and development.
Sports & Your Child's Teeth
A custom-made mouthguard is strongly advised if your child participates in sports. According to the American Dental Association, athletes who do not use one of these protection devices are 60 times more likely to suffer dental damage. A model of your child’s teeth is used to create a custom mouthguard for him or her. This will provide more protection than a store-bought model. It’s an investment that pays off handsomely in terms of reduced pain, suffering, and future dental costs!
Pediatric Dentist in Spokane Valley, WA - Top-Rated Family Dentist Near Me - Spokane Valley's Children's Dentist
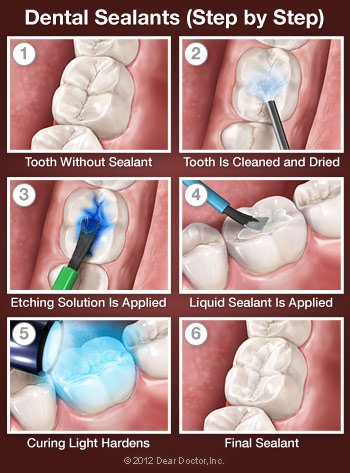 The most likely location for a cavity to develop in your child’s mouth is on the chewing surfaces of the back teeth. Run your tongue over this area in your mouth, and you will feel the reason why: These surfaces are not smooth, as other areas of your teeth are. Instead, they are filled with tiny grooves referred to as “pits and fissures,” which trap bacteria and food particles. The bristles on a toothbrush can’t always reach all the way into these dark, moist little crevices. This creates the perfect conditions for tooth decay.
The most likely location for a cavity to develop in your child’s mouth is on the chewing surfaces of the back teeth. Run your tongue over this area in your mouth, and you will feel the reason why: These surfaces are not smooth, as other areas of your teeth are. Instead, they are filled with tiny grooves referred to as “pits and fissures,” which trap bacteria and food particles. The bristles on a toothbrush can’t always reach all the way into these dark, moist little crevices. This creates the perfect conditions for tooth decay.
What’s more, a child’s newly erupted permanent teeth are not as resistant to decay as adult teeth are. The hard enamel coating that protects the teeth changes as it ages to become stronger. Fluoride, which is found in toothpaste and some drinking water — and in treatments provided at the dental office — can strengthen enamel, but, again, it’s hard to get fluoride into those pits and fissures on a regular basis. Fortunately, there is a good solution to this problem: dental sealants.
Dental sealants are invisible plastic resin coatings that smooth out the chewing surfaces of the back teeth, making them resistant to decay. A sealed tooth is far less likely to develop a cavity, require more expensive dental treatment later on, or, most importantly, cause your child pain.
How Dental Sealants Are Placed
You can think of a sealant as a mini plastic filling, though please reassure your child that it doesn’t “count” as having a cavity filled. Because tooth enamel does not contain any nerves, placing a sealant is painless and does not routinely require numbing shots. First, the tooth or teeth to be sealed are examined, and if any minimal decay is found, it will be gently removed. The tooth will then be cleaned and dried. Then a solution that will slightly roughen or “etch” the surface is applied, to make the sealing material adhere better. The tooth is then rinsed and dried again. The sealant is then painted on the tooth in liquid form and hardens in about a minute, sometimes with the help of a special curing light. That’s all there is to it!
A note about BPA: A 2012 study that received wide press coverage raised concerns that trace amounts of the chemical bisphenol-A (BPA) found in some (but not all) dental resins might contribute to behavioral problems in children. The study authors noted that while they had found an association, they had not actually proven that BPA in dental sealants causes these problems. In fact, BPA is far more prevalent in food and beverage packaging than in dental restorative materials. The American Academy of Pediatric Dentistry and the American Dental Association have since reaffirmed their support for the use of sealants.
Taking Care of Your Dental Sealants
Sealed teeth require the same conscientious dental hygiene as unsealed teeth. Your child should continue to brush and floss his or her teeth daily and have regular professional cleanings. Checking for wear and tear on the sealants is important, though they should last for up to 10 years. During this time, your child will benefit from a preventive treatment proven to reduce decay by more than 70 percent.
New parents have plenty to worry about: making sure their baby is healthy and happy, re-arranging their lives around hectic schedules and lost sleep, and figuring out what to do in all sorts of novel situations. When it comes to your child’s oral health, though, there’s plenty of help available. It all begins when you bring your youngster in for his or her first visit to the dentist.
According to the American Academy of Pediatric Dentistry, a child’s first checkup should occur by age one. Surprised? You shouldn’t be! Even though there may only be a few baby teeth visible at that age, there are plenty of things to start working on — including the development of healthy habits that will make future visits to the dentist far more pleasurable.
Unfortunately, some kids develop tooth decay at an early age. We will be on the lookout for cavities — but that’s only one reason for an early visit. Equally important is reviewing the proper ways to care for a young child’s mouth, going over your child’s developmental milestones, and discussing the importance of good oral hygiene.
Preparing for the First Dental Appointment
The way kids seem to pick up on their parents’ feelings sometimes seems uncanny; so, if you’re nervous about going to the dentist yourself, try not to let it show. Generally, this first visit involves simply talking to you and your child, looking in his or her mouth, and making oral health assessments. It’s best to tell your child what to expect beforehand, without making too big a fuss about it. You could even build some excitement by helping them get ready for “the big day.”
It’s a good idea to bring a comforting toy, a snack, and an extra diaper or two, just in case of fussiness. If possible, leave other kids at home, so the new patient can get all the attention. If not possible, bringing another adult along, however, may free your attention to focus on your child’s oral health. Likewise, filling out forms in advance may save time and effort on the day of the visit.
The Checkup
When you and your child are comfortably seated in the office, a gentle examination of your child’s mouth will be performed to uncover any early signs of dental problems such as tooth decay, and assess the risk that your child may develop the disease in the future. Often, this kind of risk assessment can help prevent — and even reverse — the early stages of tooth decay, without any drilling.
Finally, various ways to keep your child’s oral health in top condition will be discussed. This may include how diet, eating habits and oral hygiene practices can help prevent tooth decay, the most common chronic disease of childhood. That’s an important subject for everyone — even more so if your child is at greater risk. If any treatments (such as fluoride) are needed, a full explanation will be given. Tips on cleaning and brushing effectively will be reviewed and a follow-up visit will be scheduled as required.
Many habits are developed early in life. That’s why it’s important to “get it done by age one.” So when it’s time for your child’s first visit… don’t hesitate! You’ll be glad you came in.
 New parents sometimes anticipate their baby’s first tooth with a mixture of excitement and worry. While reaching a new developmental milestone is always a cause for celebration, this particular one can come with considerable discomfort. However, teething is different for each baby, and need not be painful at all; plus, there are steps you can take to make the process easier for your baby — and yourself.
New parents sometimes anticipate their baby’s first tooth with a mixture of excitement and worry. While reaching a new developmental milestone is always a cause for celebration, this particular one can come with considerable discomfort. However, teething is different for each baby, and need not be painful at all; plus, there are steps you can take to make the process easier for your baby — and yourself.
Teething refers to the process by which primary (baby) teeth emerge through the gums and become visible in the mouth. This usually begins between six and nine months of age, though it may start as early as three months or as late as one year. Usually, the lower front teeth erupt first, followed by the ones directly above. Most children have all 20 of their primary teeth by the age of 3.
Recognizing the Signs of Teething
Common signs that your baby is teething include:
- Irritability
- Biting and gnawing
- Drooling
- Chin rash (caused by excessive salivation)
- Swollen gums
- Ear rubbing
- Decreased appetite
- Disrupted sleep patterns
You are most likely to notice any of the above from about four days before the tooth breaks through the gums up until three days after the tooth appears.
A less common teething issue is the formation of an “eruption cyst,” a small bubble-like swelling filled with fluid that covers an erupting tooth. Eruption cysts usually do not require treatment as the tooth will simply pop the cyst when it comes through.
While there has been some disagreement as to whether diarrhea, rashes and fever are signs of teething, these are more likely to be associated with an unrelated illness and should be reported to your pediatrician.
How to Help
Teething babies get the most relief from cold and/or pressure on the affected area. This can be applied with:
- Chilled teething rings
- Cold, wet washcloths
- Chilled pacifiers
- Massaging baby’s gums
Make sure not to actually freeze your baby’s teething ring or pacifier because this could burn if left in the mouth for too long. The outmoded “remedy” of rubbing whiskey or other alcohol on the gums is neither effective nor appropriate. Over-the-counter medication may be helpful, but always check the correct dosage with your pediatrician or pharmacist. These, too, should not be rubbed on the gums because they can burn. Numbing agents shouldn’t be used on babies under age 2 unless directed by a physician.
Remember, it’s best to start dental visits by your child’s first birthday to establish this lifelong health-promoting routine.
 Your child’s little baby teeth have some big responsibilities. Until the adolescent years, they will not only help your youngster bite and chew (i.e., get proper nutrition) and speak correctly but also help guide the permanent teeth underneath them into proper position. In fact, a major function of baby teeth is to hold space for the adult teeth that will eventually push them out.
Your child’s little baby teeth have some big responsibilities. Until the adolescent years, they will not only help your youngster bite and chew (i.e., get proper nutrition) and speak correctly but also help guide the permanent teeth underneath them into proper position. In fact, a major function of baby teeth is to hold space for the adult teeth that will eventually push them out.
At least that’s how it’s supposed to work; sometimes, however, injury or disease can cause a baby tooth to be lost prematurely. When that happens, the permanent teeth that are coming in on either side can actually drift into the space that was reserved for another tooth. This can cause teeth to erupt out of position or to be blocked entirely, and it may result in crowded or crooked teeth.
Fortunately, if your child loses a tooth prematurely, there’s a dental appliance that can be used to hold the space open for the permanent tooth that is meant to fill it. The device is, not surprisingly, called a “space maintainer” or a “space maintenance appliance.” Made of metal and/or plastic, space maintainers can be fixed (cemented) or removable, but either way their purpose is the same: to help your child develop the best bite possible and hopefully avoid the need for braces later on.
Fixed appliances are cemented onto adjacent teeth. They are made in many different designs: One consists of a band that goes around a tooth and then a wire loop that extends out from the band to hold the space; another features a loop attached to a stainless steel crown, which goes over a nearby tooth. In either case, the loop extends just to the point where it touches the next tooth. Fixed space maintainers are often preferred with younger children, because they are less easy to fidget with, break, or misplace than appliances that can be removed.
Removable appliances look like the type of retainer that is worn at the end of orthodontic treatment. It can have a false tooth on it, which is particularly useful when the lost tooth was visible in the mouth. Older children can usually handle the responsibility of wearing this appliance and caring for it properly.
Whether fixed or removable, your child’s space maintainer will be custom-made after we take impressions of his or her mouth. A child will wear a space maintainer until x-rays reveal that the tooth underneath is ready to erupt naturally. It is very important that anyone wearing a space maintainer keep up good oral hygiene at home and have regular professional dental cleanings.
Space maintainers are also useful when one or more permanent teeth are congenitally missing — in other words, they have never existed at all. In cases like this, which are not uncommon, permanent dental implant teeth are often recommended for adolescents or adults to replace a tooth they weren’t born with. But timing is very important with dental implants — they can’t be placed in a growing child. Therefore, it is very important to use a space maintainer with a false tooth on it until jaw growth is complete and an implant can be appropriately placed. It’s a simple, non-invasive way we can avoid a malocclusion (bad bite) with some timely intervention.
 The number of children diagnosed with Attention Deficit Hyperactivity Disorder (ADHD) has been steadily increasing over the past decade. Yet according to a recent study, many children diagnosed with this condition don’t really have it; their behavioral problems are actually related to sleep-related breathing disorders (SRBD), such as sleep apnea.
The number of children diagnosed with Attention Deficit Hyperactivity Disorder (ADHD) has been steadily increasing over the past decade. Yet according to a recent study, many children diagnosed with this condition don’t really have it; their behavioral problems are actually related to sleep-related breathing disorders (SRBD), such as sleep apnea.
The 2012 study, published in the journal Pediatrics, followed more than 11,000 children for six years, starting when they were 6 months old. The children who had SRBD were 40 percent to 100 percent more likely than kids without breathing issues to develop behavioral problems resembling ADHD by the age of 7. So if your child is exhibiting ADHD-like symptoms — or has even been diagnosed with ADHD — it’s worth considering whether interrupted sleep might be an issue.
It makes perfect sense when you think about it: A well-rested individual, young or old, can function a lot better on a good night’s sleep. Yet a lack of sleep affects adults and children differently. While sleepy adults tend to act sluggish and drowsy, sleep-deprived kids are more likely to become hyperactive, uncooperative and unable to focus — just like kids with ADHD.
So what exactly is SRBD?
The condition is characterized by recurrent episodes of interrupted breathing during sleep. The child’s airway becomes blocked by soft tissues near the back of the throat — tonsils or the tongue, for example — that partially close off the windpipe. These tissues can vibrate as air passes by, causing snoring. It’s often worse while sleeping on one’s back because this encourages the lower jaw to slip back, which in turn pushes the tongue in front of the airway.
Overweight children have a higher incidence of sleep apnea due to fatty tissue deposits in the soft palate, which decrease the size of the child’s airway.
Does your child have a sleep-related breathing disorder? You can gather clues to report to your health professional by observing your child sleeping. Look for the following signs:
- Snoring
- Pauses in breathing
- Chronic mouth breathing
- Constant tossing and turning
- Night panics
- Bed-wetting
How is sleep apnea treated in children?
There are various treatments that can be very effective, depending on the cause. Enlarged tonsils and adenoids can be surgically removed. A therapy known as Continuous Positive Airway Pressure (CPAP) involves the use of a machine that delivers mild air pressure through a mask worn during sleep to keep the airway open.
Dentistry also can also play a role in treatment. For younger children who are still growing, the use of an orthodontic appliance called a palatal expander has proven helpful in some cases. A palatal expander gently widens the roof of the mouth (palate) over time by separating bones that don’t permanently fuse together until puberty. It’s most often used to create more room for crowded teeth, but the expansion can also increase airflow.
Older children who have stopped growing can sometimes benefit from Oral Appliance Therapy (OAT). This involves wearing a custom-made oral appliance designed to reposition the jaw during sleep so that the tongue is held away from the back of the throat, reducing the potential for obstruction.
The first step is to figure out what’s keeping your child from getting the restful sleep that’s so crucial to good health and well-being. For that to occur, and for your child to receive the best treatment, you will need to see a trained professional.
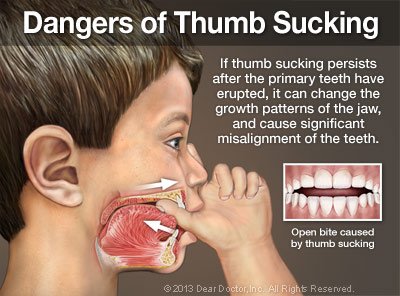 Sucking on a thumb or finger is a completely normal habit that some babies develop even before they’re born. It’s soothing, and it also helps babies make contact with and explore their environment. If sucking habits go on much past the age of 3, however, it’s possible that bite problems may arise.
Sucking on a thumb or finger is a completely normal habit that some babies develop even before they’re born. It’s soothing, and it also helps babies make contact with and explore their environment. If sucking habits go on much past the age of 3, however, it’s possible that bite problems may arise.
In a normal bite, the upper teeth grow to overlap the lower teeth. But it’s possible for the pressure of a thumb, finger or pacifier resting on the gums to interfere with normal tooth eruption and even jaw growth. Some thumb-suckers develop an “open bite,” meaning the teeth don’t overlap when a child bites together (View Example); instead, there is an open space between the upper and lower teeth. That’s why thumb sucking is definitely something we should keep an eye on, though we don’t want to intervene too soon.
Breaking the Habit
It’s important to keep in mind that most children break thumb-sucking habits on their own between the ages of 2 and 4. So if you’re trying to get your child to stop, the first thing to do is simply ignore it. Pacifiers will usually be given up more quickly than thumbs or fingers. If your child seems unable to stop when it’s time, positive reinforcements tend to work better than negative (e.g., putting a bitter substance on the thumb). Here are some things you can try:
- Praise & Reward. Explain to your child why it’s so important not to suck thumbs and think of a way to reward her for not doing it — as long as it’s not with tooth-harming sweets! Stickers or an activity they enjoy might serve well. Always offer gentle reminders rather than scold when you notice a thumb in your child’s mouth, and praise her when she stops.
- Comfort & Distract. Children have different triggers for thumb sucking. Does your child tend to do it when stressed or bored? If so, some extra hugs might help, or an activity to keep those little hands busy.
- Get Creative. You know your child best. Maybe there’s a method that would be particularly motivating to him. For example, you could tie his pacifier to a helium balloon and send it up to the Tooth Fairy. When she receives it, she can leave a special present under his pillow!
- Get Help. If your child sucks her thumb, fingers, or a pacifier, dentistry can help. Sometimes a brief conversation with a caring dental professional is all that’s needed to help her understand how it will help her teeth to kick the habit. If necessary, she can be fitted with a special oral appliance called a tongue crib (View Example), which physically prevents thumb sucking and can usually break the habit in a few months.
Thumb sucking is just one reason why it’s important to maintain your child’s regular schedule of dental exams, starting at age 1. At these appointments, you and your child can also learn effective oral hygiene techniques to help prevent tooth decay. Meanwhile, your child’s dental growth and development will be monitored. Though orthodontics can usually fix bite problems that result from sucking habits, we’d just as soon help you avoid this expense if possible!
 Some children are just too fearful to receive necessary dental care. In that type of situation, conscious sedation with nitrous oxide may be recommended to help make your child’s experience of dental treatment stress-free.
Some children are just too fearful to receive necessary dental care. In that type of situation, conscious sedation with nitrous oxide may be recommended to help make your child’s experience of dental treatment stress-free.
Nitrous oxide, a colorless gas with a slightly sweet odor, has been used in medicine for about a century. It’s a safe and effective method of administering conscious sedation, which means that a child (or adult) will stay awake during the procedure, but feel completely relaxed — even happy. All bodily functions remain normal during the administration of nitrous oxide, and its effects wear off quickly afterwards.
How Is Nitrous Oxide Administered?
As a form of conscious sedation, nitrous oxide is inhaled through a small mask that fits comfortably over a child’s nose. The gas is mixed with oxygen as it is being delivered, and both gases are always kept at a level that is safe for the body. In just a few minutes, the patient may start to experience a floating sensation, and perhaps some tingling in the hands and feet. That’s a sign that the sedation is working. Once it has been verified that your child is calm and comfortable, and that the dose is correct, the dental procedure can begin.
Nitrous oxide itself isn’t a substitute for a local anesthetic in children or adults as it’s considered an anxiolytic, which means it makes anxiety disappear. However, for some pediatric procedures, a child receiving nitrous oxide may not need an anesthetic injection. Even if they do need a numbing shot, they won’t mind at all while under sedation with nitrous oxide. Yet they won’t be asleep — they’ll be able to speak, be aware of what’s going on, and they will remain in control during the procedure. In fact, the dose can be fine-tuned to just the level of sedation they need to make them comfortable yet alert.
When the procedure is over, the flow of nitrous oxide is decreased to zero, and the oxygen will be increased. After resting in the chair for a few minutes, the child will feel completely normal.
Who Can Benefit From Nitrous Oxide?
Any child whose anxiety would preclude dental treatment can benefit from conscious sedation with nitrous oxide. Before your child is treated, you will be asked for a complete medical history, including any medications your child is taking. Your child will be kept safe and comfortable throughout the procedure, and will likely not remember a thing about it afterwards.
 Your baby’s teeth will not be visible at birth. But believe it or not, they already exist beneath the gums. Children’s primary teeth begin forming at about the sixth week of pregnancy, and start mineralizing — building the bonelike inner tooth layer (called dentin) and the super-hard enamel layer that covers it — around the third or fourth month of pregnancy. So if you’re pregnant, it’s not too early to start thinking about how to make sure your child’s teeth are as healthy as possible!
Your baby’s teeth will not be visible at birth. But believe it or not, they already exist beneath the gums. Children’s primary teeth begin forming at about the sixth week of pregnancy, and start mineralizing — building the bonelike inner tooth layer (called dentin) and the super-hard enamel layer that covers it — around the third or fourth month of pregnancy. So if you’re pregnant, it’s not too early to start thinking about how to make sure your child’s teeth are as healthy as possible!
Like everything else having to do with your baby’s physical development before birth, much depends on how well you take care of yourself. Developing teeth need certain nutrients to grow properly; if you don’t get them through your diet, your baby won’t receive them either. Likewise, you’ll have to watch your intake of substances that could harm your teeth in utero, such as certain antibiotics. Here’s a brief summary of what to seek and what to avoid.
Eat Right To Help Your Child’s Teeth Development
Certain nutrients are particularly important for prenatal tooth development:
- Calcium, a mineral, is the main component of teeth. If there is not enough calcium coming from your diet to support fetal development, your body will actually take this mineral from your bones (but not your teeth) and use it to meet your developing baby’s needs. Good for your baby, not so good for you. The best sources of dietary calcium are dairy foods such as milk, cheese and yogurt. It can also be found in broccoli and kale.
- Phosphorous, another mineral, also accounts for the hardness of teeth. It is found in every one of the body’s cells, and also in many foods — especially high protein sources such as meat and milk, but also cereals. Of all the nutrients your baby’s teeth need, this is the easiest to get.
- Vitamin D helps the body absorb and retain calcium and phosphorous. Very few foods contain it naturally — oily fish like salmon and tuna are exceptions; that’s why it is added to milk and some other beverages and foods (check labels to find out which ones). It is also produced in the body naturally when skin is directly exposed to sunlight. Concerns about the negative effects of sun exposure may prevent you from getting all the vitamin D your body requires this way, so you may be advised to take a supplement.
- Protein is the most plentiful substance in your body after water. It is responsible for building, maintaining and replacing the body’s tissues. Interestingly, it is the action of a single protein that causes calcium-phosphate crystals to form tooth enamel rather than bone. All proteins are made of amino acids, but some amino acids cannot be manufactured by the body and must come from foods. Meats and dairy products are the most protein-rich. It is possible to get all the different proteins your body requires with a vegetarian diet, but you will need to pay closer attention to what combinations of foods will provide all the essential amino acids.
Seek Guidance on Dietary Supplementation & Medications
If you feel your diet is inadequate in some nutrients during your pregnancy, it’s best to seek professional medical advice on what supplements you may need. While it’s unlikely you will ever receive too much of any given nutrient from your diet, you can overdo certain vitamins and minerals in pill form (vitamin D and calcium, for example).
When you know you’re pregnant (or if you may be pregnant), please share the news with all of your healthcare professionals who see you. That way, medications that should not be prescribed will be avoided at this time. For example, if you need antibiotics to combat an infection, some are much safer for developing babies than others. Tetracycline, for example, can permanently stain teeth in utero. Fluoride supplementation at this time is not recommended either, as there are too many unanswered questions about its use during pregnancy.

Fluoride, a naturally occurring mineral, is essential for proper tooth development and the prevention of tooth decay. In communities throughout the United States, tooth decay may still be a significant problem — but it is far less prevalent than it would have been, if not for the fluoridation of public water supplies. That’s why the major associations of pediatric dentists and doctors support water fluoridation to the current recommended levels of 0.70 parts per million (ppm). It’s also why the federal Centers for Disease Control and Prevention (CDC) has called fluoridated water one of the most significant health achievements of the 20th century.
Of course, not everyone has access to fluoridated water. That’s one reason why a fluoride supplement is often recommended for your child and/or the use of toothpastes and other products that contain this important mineral. Because it is possible for children to get too much fluoride, it is best to seek professional advice on the use of any fluoride-containing product.
Delivering Fluoride to the Teeth
Fluoride ingested by children in drinking water or supplements can be taken up by their developing permanent teeth. Once a tooth has erupted, it can be strengthened by fluoride topically (on the surface). Using a fluoride-containing toothpaste is one way to make sure your children’s teeth receive helpful fluoride exposure daily. We recommend using only a pea-sized amount for children ages 2–6 and just a tiny smear for kids under two. Fluoride should not be used on children younger than six months. A very beneficial way to deliver fluoride to the teeth is with topical fluoride applications painted right onto your child’s teeth and allowed to sit for a few minutes for maximum effectiveness.
How Much Is Too Much?
Teeth that are over-exposed to fluoride as they are forming beneath the gum line can develop a condition called enamel fluorosis, which is characterized by a streaked or mottled appearance. Mild fluorosis takes the form of white spots that are hard to see. In more severe cases (which are rare), the discoloration can be darker, with a pitted texture. The condition is not harmful, but may eventually require cosmetic dental treatment. Tooth decay, on the other hand, is harmful to your child’s health and can also be quite painful in severe cases.
The risk for fluorosis ends by the time a child is about 9 and all the permanent teeth have fully formed. Since fluoride use is cumulative, all the sources your child comes in contact with — including powdered infant formula mixed with fluoridated tap water — need to be evaluated. While caution is advised, however, it would be a mistake to forgo the benefits that this important mineral can bring to your child’s teeth — and his or her overall health.
Meet Your Top-Rated Family Dentist in Spokane Valley

Our Dental Services
Dental Crowns
Emergency Care
General Dentistry
Implant Dentistry
Orthodontics
Pediatric Dentistry
The Proof is in our Patients