Spokane Valley's #1 Oral Surgeon
You might envision a hospital stay, general anesthesia, and possibly a lengthy recovery period when you hear the phrase “surgery.” Oral surgery, on the other hand, is often a quite different experience. Oral surgery is frequently carried out in a dentist office environment and under local anesthetic, with a brief recovery period. The operations performed in oral surgery range from simple implant insertion and tooth extractions to more involved jaw realignment surgeries and emergency face trauma care.

Oral Surgery in Spokane Valley
Oral surgery procedures may be performed to relieve pain, treat an infection or trauma, restore function or improve a person’s appearance. Procedures and conditions treated include:
- Tooth Extractions. There are a variety of reasons why you may need a tooth or teeth removed. You may have a wisdom tooth that is impacted; a diseased tooth that can’t be saved; or overcrowded teeth that need to be removed so more room can be created to facilitate proper alignment during orthodontics.
- Dental Implants. Today’s preferred method of tooth replacement is a titanium dental implant, which is placed beneath the gum line and into the jawbone during a minor surgical procedure. The implant is then attached to a realistic-looking dental crown that is visible above the gum line and indistinguishable from a natural tooth.
- Oral Diagnosis & Biopsies. When a suspicious oral lesion is found, a biopsy is often used to detect or rule out oral cancer — a disease that is treatable if caught early. A biopsy involves removing a very small tissue sample for laboratory analysis.
- Corrective Jaw Surgery. Sometimes a person’s jaws don’t fit together properly. This can affect both jaw function and appearance.
- Snoring & Sleep Apnea. Excess tissue in the back of the throat may need to be removed in certain individuals with sleep apnea.
- TMD. When conservative remedies fail to relieve chronic jaw pain over a long period of time, surgery may be considered.
- Facial Trauma & Reconstructive Surgery. Facial injuries can affect not only a person’s ability to carry on basic life functions such as eating, but also his or her appearance. Knocked-out teeth can sometimes be re-implanted, or replaced with dental implants.
- Cleft Lip/Palate. These birth defects are among the most common, estimated to affect around one in 700-800 babies born in North America. With proper surgical treatment, the child has an excellent chance of leading a healthy, normal life.
What to Expect During Your Procedure
X-rays are frequently taken before oral surgery to aid in diagnosing and planning the procedure. You will be given a step-by-step explanation of your anesthetic options, and you should feel free to ask any questions you may have. The length of recovery depends on your surgical technique and general health. It’s crucial to inform your doctor about all prescription and over-the-counter medications you’re taking, as well as any lingering health issues you may have. This will help to ensure your safety and comfort, which are always of the utmost importance.
Spokane Valley's Best Oral Surgeon - Affordable Oral Surgery Near Me - Emergency Oral Surgery in Spokane Valle
 Sinus Lift Near Me
Sinus Lift Near Me
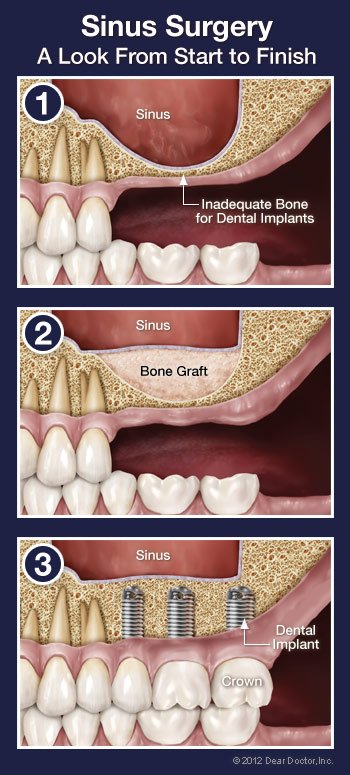
If you want to replace a missing or failing tooth with a state-of-the-art dental implant, your dentist will first need to make sure that you have sufficient bone in your jaw to anchor the implant. This is true no matter what type of tooth is being replaced. However, if it is an upper back tooth and there is not enough bone under the gum where the implant needs to go, the base of the implant could end up poking through an air space (located to the side of the nose) called a sinus cavity. Since you can’t anchor a dental implant to air, this presents a problem — but it is one that can often be solved with a minor in-office surgical procedure called a “sinus membrane lift.”
A sinus membrane lift, or sinus augmentation, involves adding bone to fill in the bottom of that air space, essentially raising the floor of the sinus cavity. Why wouldn’t there be enough bone there already? For some people, it’s simply a matter of how large their sinus cavities are, and their shape. In other cases, bone has actually been lost from the area. For example, if your tooth has been missing a long time, the bone that used to surround it may have begun to deteriorate. Bone in general needs stimulation to stay strong; in the case of the jawbone, that stimulation comes from the teeth. When teeth are lost, the bone loses stimulation and the body ceases to make new bone cells in that area. This leads to a reduction in bone volume and density. Also, if your tooth loss was due to periodontal (gum) disease, your tooth-supporting bone may have been reduced as a result of the disease. No matter what the reason is for insufficient bone, a sinus membrane lift can create more bone where it is needed.
Where does this additional bone come from? It can be bone from elsewhere in your body, such as another part of your jaw or your hip. But most often, it will be bone-grafting materials that are processed in a laboratory for these kinds of purposes. The original source may have been a human or animal donor (usually a cow). Synthetic products can also be used. All grafting materials must be approved by the Food and Drug Administration (FDA) and prepared according to their guidelines. The materials are specially treated to render them completely sterile, non-contagious, and free of rejection factors. For the most part, bone grafts act as scaffolds that the body will eventually replace with its own bone.
The Sinus Lift Procedure
Prior to scheduling surgery, your dentist will assess the shape, location, and health of the sinus using x-ray imaging. Your options for anesthesia will also be discussed. The surgery itself is usually carried out under local anesthesia by numbing the area, just as is done for a routine filling. Some people require additional sedation or anti-anxiety medication, which can either be administered orally (by mouth) or by intravenously (through a vein) via injection.
When the area has been completely numbed, an incision will be made in your gum to expose the bone that used to contain your missing tooth or teeth. A small opening will be made in the bone to reveal the membrane that lines the sinus. This membrane will be raised and the space beneath it will be filled with bone grafting material. The gum is then stitched back up. In some cases, the implant(s) can be placed directly into the grafting material before the gum is closed, eliminating the need for a second surgical procedure later on to place the implant. Often, however, the surgical site is allowed to heal for approximately 6-7 months before an implant is placed.
What to Expect After Sinus Surgery
You may experience moderate swelling and some minor discomfort that generally lasts a few days — about the same as having an upper impacted wisdom tooth removed. Sometimes a non-steroidal anti-inflammatory medication (prescription or over-the-counter) is recommended to help minimize this. A course of antibiotics may be prescribed to prevent infection. If the sinus membrane becomes a bit inflamed, leading to a feeling of minor congestion, a decongestant can be helpful. If you suffer from seasonal allergies, make sure to schedule your surgery for a time when this will not be an issue.
 Oral Cancer Screening in Spokane Valley
Oral Cancer Screening in Spokane Valley
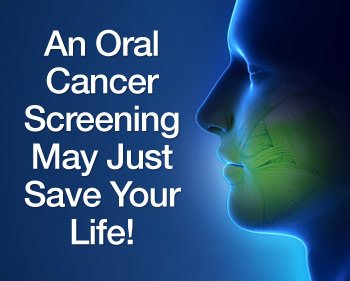
Although oral cancer may not get as much attention as some more widely-known types of cancer, that doesn’t mean it’s any less deadly. In fact, it is estimated that in the United States, oral cancer is responsible for killing one person every hour, every day. While it accounts for a relatively small percentage of all cancers, oral cancer is dangerous because it isn’t usually detected until it has reached an advanced stage. At that point, the odds aren’t great: only about 6 in 10 people will survive after five years of treatment.
If there was a simple test that could give you an early warning about whether you’re likely to have this disease, would you take it? The good news is — there is! Since early detection has been shown to increase the survival rate of oral cancer to 80% or better, this test can truly save lives. And best of all, having an oral cancer screening is part of something you should be doing anyway: getting regular dental checkups.
An oral cancer examination is fast and painless. Its objective is to identify small changes in the lining tissues of the mouth, lips and tongue that may signify the early stages of this type of cancer. The screening is primarily a visual and tactile (touch) examination. If any abnormalities are noted, a small tissue sample can be retrieved for further testing in a laboratory.
Who’s At Risk for Developing Oral Cancer?
The answer might surprise you. Oral cancer used to be thought of as an older person’s disease, and it still mostly affects those over 40. But today, younger people form the fastest-growing segment among oral cancer patients. This is primarily due to the spread of the sexually-transmitted Human Papilloma Virus (HPV16).
Of course, the other major risk factors still apply: If you’re middle aged or older, a moderate to heavy drinker or a long-time tobacco user, you have a greater chance of developing oral cancer. Chronic exposure to the sun, long known to cause skin cancer, is also associated with cancers of the lips. Genetic factors are thought to have a major impact on who gets the disease as well.
Detecting Oral Cancer
A thorough screening for oral cancer is part of your routine dental checkup — another reason why you should be examined regularly. The screening includes a visual assessment of your lips, tongue, and the inside of your mouth, including a check for red or white patches or unusual sores. You may be palpated (pressed with fingers) to detect the presence of lumps and swellings, and your tongue may be gently pulled aside for an even better view. A special light, dye, or other procedure may also be used to help check any suspect areas. If anything appears to be out of the ordinary, a biopsy can be easily performed.
If you notice abnormal sores or color changes in the tissue of your mouth, lips and tongue, they may be a symptom of oral cancer — most, however, are completely benign. But sores or other unusual changes that haven’t gone away by themselves after 2-3 weeks should be examined. Remember, the only way to accurately diagnose oral cancer is through a laboratory report. Early diagnosis, aided by thorough screenings at your regular dental checkups, is one of the best defenses against oral cancer.
 Wisdom Tooth Removal
Wisdom Tooth Removal
In most people, the third set of molars, generally called “wisdom teeth,” start coming in around age 17-25. However, the arrival of these teeth is often far from trouble-free. The extraction (removal) of one or more third molars is a relatively common procedure, performed on some 5 million patients every year. After a thorough examination and diagnostic tests such as x-rays or a CT scan, you may be told that you should have your wisdom teeth extracted. Here are some typical reasons why:
- Your jaw may be too small to accommodate all your teeth, leading to excessive crowding and the chance of your wisdom teeth becoming impacted — that is, unable to emerge from the gums, and potentially harmful to adjacent bone or teeth
- Your wisdom teeth may be erupting (coming in) in a crooked orientation, which can damage other teeth or anatomical structures in the jaw, and/or cause bite problems
- If your wisdom tooth does not fully erupt (emerge from the gums), it can increase the chance for bacterial infection
- A cyst (a closed, fluid-filled sac) may develop around the unerupted wisdom tooth, which can cause infection and injury to the adjacent bone or nerve tissue
Whether it is aimed at preventing future problems or needed to alleviate a condition you already have, the extraction of wisdom teeth can be an effective treatment. But, as with all medical procedures, its benefits must be weighed against the small risk of complications, and should be discussed in detail.
The Extraction Procedure
Wisdom tooth extraction is usually an in-office procedure which may be performed by a dentist or an oral surgeon. It’s quite possible to have the treatment done with only a local anesthetic (numbing shot) to keep you from experiencing any pain; however, if multiple teeth are being extracted at one time (as is often the case), a general anesthetic or conscious sedation may be administered. The type of anesthesia that’s best for you will be determined before the procedure.
Once you have been appropriately anesthetized, the gum tissue at the extraction site may need to be opened if the tooth is impacted. The tooth itself will then be gently removed. When the extraction is complete, you may need to have the site sutured (stitched) to aid healing. After the procedure is over, you will rest for a short time before going home. Depending on what type of anesthesia you have had, you may need another person to drive.
After the Procedure
The recovery period after wisdom tooth extraction generally lasts only a few days. During this time, you should rest when possible to encourage healing, and take any pain medication as prescribed. It’s normal to experience some bleeding at the extraction site; this can be controlled by gently biting on gauze pads, changing them as needed, and resting with the head elevated on pillows rather than flat.
Holding an ice pack on the outside of your cheek for a few minutes at a time (for example, 5 minutes on / 5 minutes off) may help reduce swelling on the first day after the procedure. Starting on day 2, the warm moist heat of a washcloth placed on the cheek may make you more comfortable. Rinsing the mouth with warm salt water a few times a day can also help relieve discomfort.
You may want to eat soft foods for a few days after the extraction; likewise, be careful when brushing or putting anything in your mouth until your healing is complete. Be sure to follow the postoperative instructions you are given, as each situation is a little different; this will help you to be as comfortable as possible.
 When you were a youngster, did you ever get a black eye, chip a tooth or bruise your cheek? If so, you may have experienced a case (let’s hope, a mild one!) of facial trauma. In many situations, however, facial trauma can be severe. Among its major causes are auto accidents, sports injuries, work-related mishaps, falls, and acts of violence. When serious facial injury occurs, it’s important that you receive immediate and comprehensive care. That’s why oral and maxillofacial surgeons are on call at most emergency and trauma centers.
When you were a youngster, did you ever get a black eye, chip a tooth or bruise your cheek? If so, you may have experienced a case (let’s hope, a mild one!) of facial trauma. In many situations, however, facial trauma can be severe. Among its major causes are auto accidents, sports injuries, work-related mishaps, falls, and acts of violence. When serious facial injury occurs, it’s important that you receive immediate and comprehensive care. That’s why oral and maxillofacial surgeons are on call at most emergency and trauma centers.
Facial trauma in general involves injuries to the soft- or hard-tissue structures of the face, mouth or jaws — including the teeth, the bones of the jaws and face, and the tissue of the skin and gums. It can also involve treatment of particular specialized regions, such as the area around the eyes, the salivary glands or facial nerves. Because facial injuries can affect not only a person’s ability to carry on basic life functions (eating, vision, etc) but also his or her appearance, there is often a strong emotional component to treatment as well as a physical one. But after completing an extensive training program, oral and maxillofacial surgeons are capable of handling the full scope of facial injuries.
Treatments for Facial Injury
Some facial traumas are relatively minor. A common one occurs when a tooth is loosened or knocked out (avulsed). Many times, if treated immediately, the tooth can be successfully re-implanted in the jaw. If that isn’t possible, placing a dental implant is often the most effective way to replace a missing tooth.
Another type of relatively common but more serious injury may involve a fracture of the facial bones, including the cheekbones, upper or lower jawbones, or the eye sockets. In principle, its treatment is essentially the same as that used for a broken arm: place the bones back in their proper position, and immobilize them. But since it isn’t possible to put a cast on the face, different immobilization techniques are used. One method involves wiring the upper and lower jaws together to let them heal in the correct alignment; alternatively, plates and screws may be used to permanently reattach the bones.
Severe facial trauma is often a critical condition, since over 60% of these patients also have serious injuries in other parts of the body. In fact, many of the standard techniques used in trauma centers were developed by oral and maxillofacial surgeons during the wars in Korea, Vietnam, and the Middle East. Restoring breathing, controlling bleeding and checking for neurological damage are top priorities. After that, as much of the reconstructive surgery as possible is accomplished in one operation.
Preventing Facial Trauma
What’s the best treatment for facial trauma? Prevention. Always wearing seat belts, using proper helmets and protective gear when playing sports, and staying out of dangerous situations (like driving while impaired, tired or distracted) can go a long way toward keeping you safe. If you’re engaging in athletic activities that carry any risk of facial injury, wear a properly fitted mouthguard — this small piece of protective equipment can save you a lot of potential harm.
But if you (or someone you care for) require a trip to the emergency room for a facial injury, be sure to ask for a consultation with an oral and maxillofacial surgeon, so that you get the best care and the most favorable outcome.
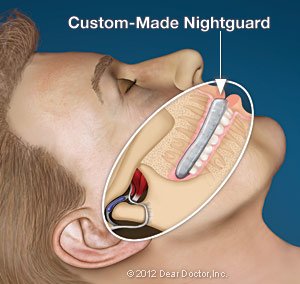 People don’t generally think of a dentist as the healthcare professional to see for recurring headaches or migraines; yet dentists can play a role in diagnosing and even treating your condition. That’s because quite often, recurring pain that is felt in the area of the temples on the sides of the head is actually caused by unconscious habits of clenching and/or grinding the teeth. These habits, which often manifest during sleep, put tremendous pressure on the muscles that work your jaw joint, also called the temporomandibular joint (TMJ).
People don’t generally think of a dentist as the healthcare professional to see for recurring headaches or migraines; yet dentists can play a role in diagnosing and even treating your condition. That’s because quite often, recurring pain that is felt in the area of the temples on the sides of the head is actually caused by unconscious habits of clenching and/or grinding the teeth. These habits, which often manifest during sleep, put tremendous pressure on the muscles that work your jaw joint, also called the temporomandibular joint (TMJ).
The fan-shaped temporalis muscles located over your temples on either side of your head are two of several muscles involved in jaw movement. You can easily feel them working if you put your fingertips on your temples while clenching and unclenching your jaw. When temporalis muscles go into spasm from too much clenching, headache symptoms may result. This is not to say that headaches and migraines are always caused by TMJ problems, also known as temporomandibular disorders (TMD). But given the established link between them, it definitely bears looking into — especially if a diagnosis remains elusive in your case.
Sources of Relief
The first thing you need is a thorough oral exam to determine if there is evidence of a clenching or grinding (also known as “bruxing”) habit or TMD. If so, there are things you can do for immediate and long-term relief. Sometimes eating softer foods for a few days can reduce stress on the muscles and joints. Ice and/or moist heat can help relieve soreness and inflammation. Gentle stretching exercises, non-steroidal anti-inflammatory medications such as ibuprofen, and muscle relaxants can also provide relief.
Finally, a custom-made nightguard to wear when you sleep might be recommended. This plastic oral appliance, which fits over the teeth, can control or even eliminate clenching and grinding, reducing pressure on the muscles that work the jaw and the jaw joint itself. Some users have reported that their headaches or even migraines are less frequent and/or less intense.
Will a nightguard or other TMD therapy relieve your headaches? It depends on the source of the problem. But living with chronic headaches or facial pain is no fun — so don’t delay scheduling an exam and a consultation.
 Cleft lip and cleft palate are among the most common birth defects, estimated to affect around one in 700-800 babies born in North America. Both problems result from the incomplete formation of anatomical structures (the lips and the palate, or “roof of the mouth”) which develop during early pregnancy. These conditions may occur separately or together, and they can have a wide variation in severity. With proper treatment, however, in most cases the child has an excellent chance of leading a healthy, normal life.
Cleft lip and cleft palate are among the most common birth defects, estimated to affect around one in 700-800 babies born in North America. Both problems result from the incomplete formation of anatomical structures (the lips and the palate, or “roof of the mouth”) which develop during early pregnancy. These conditions may occur separately or together, and they can have a wide variation in severity. With proper treatment, however, in most cases the child has an excellent chance of leading a healthy, normal life.
Besides the noticeable irregularity in appearance, a cleft lip or palate can cause difficulties with feeding and speech. Both conditions are also associated with ear infections, hearing loss and dental problems. To fully address these problems, a child may require several surgical procedures, performed at different times. That’s why a team approach is often used to treat this complex condition. Members of the medical team may include an oral surgeon, a pediatric dentist, an orthodontist, a plastic surgeon, and other specialists.
In general, the first goal of treatment is to repair or “close” the gap in the lip and/or palate as soon as it is practical for the child — as early as 2 to 9 months of age. Follow-up treatment may be needed to restore the appropriate form and function of the lips, teeth, and jaws (for proper speech, eating, etc) and to correct hearing problems. These procedures may include plastic surgery, orthodontics, orthognathic (jaw) surgery and speech therapy.
Surgical Treatment for Cleft Lip or Palate
Cleft lip or palate surgery is usually performed in a hospital setting, and may be done when an infant is 6 to 12 weeks old. Intravenous sedation or general anesthesia is used, so your child won’t experience any pain. In cleft lip surgery, an incision is typically made on each side of the cleft. This creates several “flaps” of tissue, which are then sutured (stitched) together to close the gap. Suture lines are generally planned to follow the facial contours, so that the surgical scar will be as unobtrusive as possible.
Cleft palate treatment involves rebuilding the roof of the mouth, including soft tissue, muscle and bone. The initial surgery is often performed between the ages of 6 and 18 months. Like cleft lip surgery, it relies on specialized “flap” techniques to reposition soft tissues and close the gap. Before or after surgery, your child may need to wear a special appliance such as an obdurator (artificial palate) or a nasal alveolar molding device (NAM), a type of retainer.
Follow-Up Treatment
Depending on how complex the child’s condition is, additional procedures may be required after the initial treatment to fully correct any defects. A child’s treatment plan will often include pediatric dental examinations beginning around age one. Bone grafts to repair the hard palate may be recommended at age 8-11 years, when the cuspid teeth are developing. To correct problems with the alignment of teeth, orthodontic care may be needed beginning around age 12. In some situations, orthognathic surgery is recommended to address more severe jaw problems.
Handling a child’s cleft lip or palate can be a challenge for caregivers and family members — but it’s important to keep in mind that this relatively common birth defect can be successfully treated. Many who have this condition have gone on to become well-known performers, politicians, sports stars… as well as moms and dads, friends and neighbors.
 The main goal of dentistry is to preserve your natural teeth and keep them healthy for as long as possible. There are times, however, when it is in your best interest (or your child’s) to have a tooth extracted (removed). This could be the case for a variety of reasons. Perhaps you have a tooth that has been severely damaged by trauma or decay; or an impacted wisdom tooth that may cause trouble for you later on. Maybe your teenager will soon undergo orthodontic treatment and has insignificant space for his adult teeth, referred to as crowding. Or your younger child has a baby tooth that’s stubbornly adhering, even though it’s past time for it to go.
The main goal of dentistry is to preserve your natural teeth and keep them healthy for as long as possible. There are times, however, when it is in your best interest (or your child’s) to have a tooth extracted (removed). This could be the case for a variety of reasons. Perhaps you have a tooth that has been severely damaged by trauma or decay; or an impacted wisdom tooth that may cause trouble for you later on. Maybe your teenager will soon undergo orthodontic treatment and has insignificant space for his adult teeth, referred to as crowding. Or your younger child has a baby tooth that’s stubbornly adhering, even though it’s past time for it to go.
Whatever the reason, tooth extraction is more often than not a very routine procedure. How straightforward this minor surgery is will depend on where the tooth to be extracted is located in the mouth, and what its roots are like. For example, a front tooth with a single straight root is easier to remove than a molar with multiple roots. This is especially true when that molar is a wisdom tooth that is impacted, meaning it is below the surface surrounded by gum tissue and bone. Often, a wisdom tooth is blocked from fully erupting (growing in) by other teeth in its path.
Still, tooth extraction is nothing to be feared when done by an experienced hand. Keep in mind that a tooth is not rigidly fixed in its surrounding bone, though that’s how some may picture it. In fact, it is attached to the bone via a network of fibers that form what’s known as the periodontal ligament. By carefully manipulating the tooth, these fibers can be detached and the tooth freed without much trouble.
Reasons for Extracting a Tooth
As mentioned above, there can be a variety of reasons for extracting a tooth. Be sure to ask questions about the pros and cons of any dental treatment, including extraction.
- Trauma or Disease — In both of these situations, there are several ways to try and save the tooth. The damaged tooth might need a full-coverage crown, a root canal treatment, or both. But sometimes even these methods are not enough to keep the tooth functioning well and looking good; it might be better to remove the tooth and replace it with a strong and lifelike dental implant.
- Orthodontic Treatment — Teeth are sometimes extracted when there are too many of them for the size of the dental arches (jaws), a situation known as crowding. After an adequate amount of space is opened up through the extraction of one or more teeth, the remaining teeth can be aligned properly. The teeth most frequently removed for orthodontic reasons are the first premolars, which are right next to the eyeteeth (canines).
- Impacted Wisdom Teeth — Early removal of impacted wisdom teeth can prevent damage to neighboring healthy teeth, bone, gum tissue, even nerves and blood vessels. If an impacted wisdom tooth is in a bad position, it’s best to remove it before its roots are fully formed.
- Baby Teeth — If a baby tooth is out of position or not lost in the right sequence, the permanent tooth underneath it might not erupt normally. In this case, removing the baby tooth could prevent a need for orthodontic treatment later on.
The Process of Extracting a Tooth
The first step in any extraction is a radiographic (x-ray) examination to assess the position of the tooth roots and the condition of the surrounding bone. This will allow any possible complications to be anticipated. A thorough medical and drug history is taken, to ensure that you are healthy enough to undergo the procedure, and your options for anesthesia will be discussed.
Tooth extraction is usually carried out with local anesthesia, which will numb the teeth to be removed, and the surrounding bone and gum tissues. Additional sedatives might also be used, including oral sedatives (taken in pill form), nitrous oxide (which is inhaled) and/or conscious sedation, which is given intravenously (into a vein). The latter is usually required for more complicated (or multiple) tooth extractions. By the time the sedation medication has worn off, you won’t even be aware that the surgery was done.
As your tooth is being removed, steps are taken to ensure the bone that surrounds it isn’t damaged. Sometimes, in the process of removing a tooth, a small amount of lab-processed bone-grafting material is placed into the socket to help preserve the bone volume there. This is particularly important when the extraction is going to be followed at some point by the placement of a dental implant, which needs to fuse to existing bone, or orthodontics, which gently moves teeth through bone.
What to Expect After Tooth Extraction
Immediately after your tooth is extracted, the socket will be covered with sterile gauze; gentle pressure will be applied for 10-20 minutes to control any bleeding. Small sutures (stitches) might also be used for this purpose. It’s normal to experience some mild to moderate post-operative discomfort and/or swelling. Taking non-steroidal, anti-inflammatory drugs such as ibuprofen and/or aspirin the day of surgery should control most symptoms. Antibiotics may also be prescribed to ensure infection-free healing. Using ice packs on the outside of your jaw, and eating softer foods until you feel more comfortable can also be helpful. Within a few days, all should be back to normal.
 There’s so much dentistry can do these days to make your mouth healthier and your smile more beautiful. Yet many people don’t take advantage of this because of a long-standing fear of dental treatment. If you are one of these people, rest assured that it’s possible to have an experience that’s free of anxiety and pain. This can be accomplished by blocking your sensations of pain with local anesthetics or by giving you medication that can help you relax. Sometimes both are needed to ensure maximum comfort, especially if you are someone for whom the injections that deliver local anesthetics are themselves a major source of anxiety.
There’s so much dentistry can do these days to make your mouth healthier and your smile more beautiful. Yet many people don’t take advantage of this because of a long-standing fear of dental treatment. If you are one of these people, rest assured that it’s possible to have an experience that’s free of anxiety and pain. This can be accomplished by blocking your sensations of pain with local anesthetics or by giving you medication that can help you relax. Sometimes both are needed to ensure maximum comfort, especially if you are someone for whom the injections that deliver local anesthetics are themselves a major source of anxiety.
When you are afraid of dental treatment, your guard goes up and your pain threshold goes down; anticipating that something will hurt makes you hypersensitive to every sensation — even sound. If this describes your experience in the dental chair, then you might benefit from sedatives that can be given during your visit to make that anxiety melt away.
Before any particular sedative is recommended, you will be asked to provide your complete health history, including any medications you are currently taking — both prescription and over-the-counter. It is also important to know if you smoke or drink. On the day of your treatment, you may need to have someone drive you to and from your appointment as certain medications take time to wear off.
Ways to Relieve Anxiety
Oral Sedation — Oral sedation (given by mouth) is a popular option for many people precisely because it does not require the use of needles. Oral sedatives are either swallowed whole in pill form or can be dissolved under the tongue. Both methods work in a matter of minutes. A variety of oral sedative and anxiolytic (anxiety-dissolving) medications have been developed through extensive research and testing to make your experience of dental treatment as comfortable and relaxing as possible. All have long safety records after decades of use, and several even have “amnesic” properties, meaning you will remember little to nothing, even though you are conscious throughout the treatment. Commonly prescribed medications include Valium®, Halcion®, Sonata®, Ativan®, Vistaril®, and Versed®.
Inhalation Conscious Sedation — Nitrous oxide, a sedative you inhale, has been used in dental offices for nearly 100 years. It is a relatively poor pain reliever but a very good anti-anxiety medication. It is administered through a nasal hood, which resembles a small cup that is placed over your nose. The oxygen mixed with nitrous oxide provides a light-headed or even euphoric feeling, which is quick to wear off so there is no “hangover” effect. All bodily functions remain essentially normal during the use of this sedative, which is very safe.
IV Conscious Sedation — Sedatives delivered directly into the bloodstream intravenously (into the vein) are more potent than when taken orally, and the amnesic effects may be more profound. Because IV sedation has an almost immediate effect on the body and its functions — including heart rate, blood pressure and breathing — there is a higher degree of risk associated with it than with other types of sedatives. There is also a higher level of training required for those who administer it. As with all sedation (except nitrous oxide), you must be monitored with specialized equipment throughout your IV sedation treatment. The main advantage is that drugs administered this way work immediately and the level of sedation can be adjusted more quickly and easily. And with most sedatives, you won’t remember a thing about your dental procedure after the sedative wears off.
 Do you think of bone as a hard, rigid material that never changes? In fact bone remodels itself all the time: Your body is constantly depositing new bone cells and removing old ones. In the case of the bone that supports your teeth, this process can be helpful or harmful. For example, the jawbone’s adaptability allows an orthodontist to move teeth into a better position with braces. But in the case of losing a tooth as an adult, the bone changes that result can have serious consequences.
Do you think of bone as a hard, rigid material that never changes? In fact bone remodels itself all the time: Your body is constantly depositing new bone cells and removing old ones. In the case of the bone that supports your teeth, this process can be helpful or harmful. For example, the jawbone’s adaptability allows an orthodontist to move teeth into a better position with braces. But in the case of losing a tooth as an adult, the bone changes that result can have serious consequences.
When teeth are lost, the bone that used to surround them begins to melt away or “resorb.” Tooth-supporting bone can also be lost when you have periodontal (gum) disease. If you loose enough teeth and bone, your facial features will sag, giving you a more aged appearance; it can also complicate treatment to replace your missing teeth. Fortunately, with modern bone grafting-techniques, the bone that has been lost can be built up again. This can benefit both your health and appearance by strengthening your jawbone, allowing more effective tooth replacement, and increasing support to your facial features.
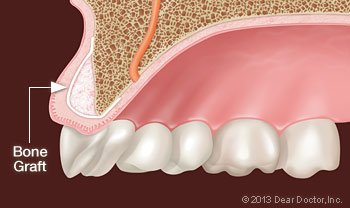
Bone grafting is a minor surgical procedure that is normally done in a dental office. An incision is made in your gum to gain access to the bone beneath it, and then grafting material is added. Most often, the grafting material is processed bone minerals around which your body will actually deposit new bone cells.
The grafting material itself can come from your own body, but very often it is bone from an animal or human donor that has been treated by a laboratory to make it sterile and safe. It can even be a synthetic substance. Grafting material comes in a variety of forms: powder, granules, putty or a gel that can be injected through a syringe. The graft, which is generally covered by a collagen membrane for optimum bone repair, will act as a scaffold onto which your body will build new bone.
Uses for Bone Grafts
Bone grafts are used in dentistry to accomplish the following treatment goals:
- Saving Teeth — When severe periodontal disease causes bone loss, teeth can become loose and at risk of being lost. In order to save them, the bone around them can be regenerated through grafting; this increases bone support and helps keep them in place.
- Tooth Extractions — These days, it is very common to deposit bone grafting material into a tooth socket after a tooth has been removed. That way, should you want to replace your tooth with a dental implant later on, that option will be available.
- Dental Implants — In this optimal tooth-replacement system, a small titanium post embedded in the jawbone is attached to a highly realistic dental crown, permanently replacing the missing tooth. Implants require good bone volume and density to achieve their excellent functionality and high success rates. If you have already experienced bone loss, a graft can help regenerate enough bone to place the implant successfully.
What to Expect from Bone Grafting
The procedure for placing a bone graft usually requires only local anesthesia, though oral or IV (intravenous) sedatives can also be used to achieve a higher state of relaxation. Since a small incision is made in your gum tissue to gain access to the bone that will receive the graft, you may experience some soreness in the area after the surgery. This can usually be managed by over-the-counter anti-inflammatory medication and/or pain relievers, as well as ice therapy after the procedure. Any discomfort should only last a day or two. Then, over the next several months, your body will replace the graft with its own bone, reversing the decline in bone quantity you have experienced.
 Millions of people regularly take anticoagulant or antiplatelet medications (sometimes called “blood thinners”) to help prevent heart attack and stroke, and to manage a variety of medical conditions including cardiac arrhythmia and stent placement. While these drugs have proven, life-saving benefits, they can also cause side effects such as increased bleeding. So it may be a cause for concern if you’re taking one of them and you need to have a dental procedure.
Millions of people regularly take anticoagulant or antiplatelet medications (sometimes called “blood thinners”) to help prevent heart attack and stroke, and to manage a variety of medical conditions including cardiac arrhythmia and stent placement. While these drugs have proven, life-saving benefits, they can also cause side effects such as increased bleeding. So it may be a cause for concern if you’re taking one of them and you need to have a dental procedure.
Anticoagulants are among the more widely used pharmaceuticals today, particularly for heart patients. Some common prescription anticoagulants include heparin, warfarin (Coumadin and generics), clopidogrel (Plavix) and dabigatran etexilate (Pradaxa). Regular aspirin and NSAIDS (like Advil) also have anticoagulant properties. The purpose of anticoagulant medications is to keep the blood from clotting (clumping together) as readily as it normally does; this reduces the chance of a clot forming inside a blood vessel, which could lead to a stroke or heart attack.
If you are taking one or more of these medications, it will take longer for any type of bleeding to stop. For some dental or surgical procedures, that’s a factor that must be considered. The most important thing you should do is inform your dentist right away if you are taking any kind of anticoagulant or antiplatelet medication — especially if you have just started taking it. The name and dosage of your medication will be noted in your records, and your cardiologist (or other specialist) will be consulted if necessary, to determine what’s best for you.
Having Dental Work with Blood Thinners
While each patient is different, there are some generally accepted guidelines for having dental work while taking anticoagulant medications. If the drug is being taken on a temporary basis (after knee replacement, for example) then the safest choice might be to put off non-essential dental procedures. However, in many cases it’s entirely possible to have needed work done while taking anticoagulants. In each situation, the risk of increased bleeding must be balanced against the chance that going off the medication could cause more serious problems.
A number of studies have shown that for many common dental procedures — cleanings, fillings and restorations, for example — it’s safer to continue taking anticoagulant medications than to stop, even temporarily. That’s because it is generally possible to control bleeding with local measures (such as biting down on gauze), using hemostatic devices and minimally invasive surgical techniques. Scheduling dental work for early in the day and allowing plenty of time for rest afterwards also provides an opportunity to control any bleeding that does occur.
More Complex Procedures
In some cases, more extensive dental procedures such as tooth extraction or implant placement may be recommended for people taking anticoagulants. As always, the potential risks and benefits of stopping the anticoagulant medication must be carefully weighed. To help in the decision-making process, one or more diagnostic blood tests, such as prothrombin time (PT) or International Normalized Ratio (INR), may be ordered. Then a judgment can be made, based on the test results and on clinical experience.
While it’s extremely rare for common dental procedures to cause potentially life-threatening complications, it makes sense to take as few chances as possible. That’s why you should tell us about any medications you may be taking, including herbs and vitamins. While taking anticoagulants doesn’t prevent you from having dental work, it’s important to share information about your medications so you can get the best results from your treatment.
 When you come into the dental office for an examination, you might assume that the focus is on your teeth. That’s often correct — but don’t forget that there are a number of other parts of the oral and facial anatomy that are examined as well. These include areas around and inside the mouth (such as the lips, gums, hard and soft palate, and the tongue) as well as outside the mouth (the skin, muscles and glands in the neck, and the temporomandibular joint). In fact, when it comes to detecting certain oral or systemic (whole-body) diseases, a thorough dental exam may be your first line of defense.
When you come into the dental office for an examination, you might assume that the focus is on your teeth. That’s often correct — but don’t forget that there are a number of other parts of the oral and facial anatomy that are examined as well. These include areas around and inside the mouth (such as the lips, gums, hard and soft palate, and the tongue) as well as outside the mouth (the skin, muscles and glands in the neck, and the temporomandibular joint). In fact, when it comes to detecting certain oral or systemic (whole-body) diseases, a thorough dental exam may be your first line of defense.
How are diseases in the mouth discovered? Most of the time, it’s simple: You will be asked about any changes you have noticed, or symptoms you may be experiencing. Your face, mouth, and neck will then be visually inspected, and certain areas may be palpated (gently touched or pressed with fingers) or probed (touched with a small instrument). If needed, additional tests or diagnostic imaging (X-rays or other methods) may be used to aid in diagnosis.
Occasionally, an abnormality such as a lesion (an unusual localized change in your tissues) is found that needs to be examined further. Lesions may resemble white or red spots or lumps (tumors), but they are typically benign. However, it is often better to err on the side of caution and perform a biopsy to be sure. This may involve making a small incision and removing a part of the suspicious area. The tissue sample will be sent to a pathologist, who examines it under a microscope for signs of disease.
Some Oral Diseases To Look For
Oral cancer is perhaps the most significant disease to look for in an examination — both because it can be life-threatening, and because early detection is proven to increase the survival rate. But it’s important to remember that a large majority of unusual growths are found to be benign. Some other oral diseases that may be screened for include:
- Fibroma, a thickened mass that may feel like a lump in the lining of the mouth.
- Leukoplakia, a condition that causes white patches to form inside the mouth. While usually benign, the lesions may be precancerous and are often biopsied.
- Lichen Planus, an inflammatory disease that sometimes causes discomfort.
- Mucous Membrane Pemphigoid, an autoimmune disease that may cause oral lesions, but is not life threatening.
- “Pregnancy Tumors,” benign red swellings that may form on gum tissue of pregnant women due to hormonal changes.
In addition, some systemic diseases (such as diabetes, Crohn’s disease, and heart disease) may produce effects that can be observed in the mouth. We are always on the lookout for signs of these potentially serious conditions.
When a Biopsy Is Needed
Although the majority of oral lesions are benign, if there is any possibility that the growth could be cancerous or pre-cancerous, it’s likely that a biopsy will be performed. Depending on how much tissue needs to be removed, this may be a simple in-office procedure, or it may be done in a hospital setting. Typically, the procedure requires only local anesthesia, and it doesn’t take long. If incisions are made, they are often closed with self-dissolving sutures (stitches) that don’t need to be removed.
Because the oral tissues are rich in blood vessels, some bleeding is normal for a period of time afterward. You will be given follow-up instructions as needed, including how to manage swelling and discomfort, when to take medication, and what to eat and drink. Getting some rest and maintaining good oral hygiene will also help you get back to normal as quickly as possible. When the pathology report is complete (usually in a few days), you will be given the results.
In many cases, problems with the bite or the alignment of the teeth can be corrected using today’s advanced methods of dental and orthodontic treatment. Sometimes, however, skeletal and dental irregularities aren’t so easy to remedy, even with the most up-to-date non-surgical techniques. That’s when corrective jaw surgery (also called orthognathic surgery) may be recommended.
While it may sound like a complex and demanding treatment, jaw surgery isn’t always so serious. It’s often performed as a routine in-office procedure — for example, to extract impacted wisdom teeth (molars that don’t fully protrude through the gums), or to place dental implants in the jaw. However, it can also be used to remedy severe orthodontic problems involving the relationship between the teeth and jaws, including the correction of underbites (the most frequent surgical correction) and congenital abnormalities (birth defects) related to jaw development. It can even help alleviate sleep apnea, a potentially life-threatening condition.
Who Can Benefit From Jaw (Orthognathic) Surgery
People who have problems related to the jaws, tooth alignment and facial asymmetries, which create difficulties chewing, talking, sleeping, or carrying on routine activities, may benefit from having orthognathic (jaw) surgery. These procedures can also be used to correct aesthetic issues, such as a protruding jaw, a congenital defect, or an unbalanced facial appearance.
After a thorough examination, it can be determined if you’re a candidate for orthognathic surgery. In general, if orthodontic treatment can solve the problem, that’s where you will start. Yet, while orthodontics can successfully align the teeth, it’s sometimes the jaws themselves that need to be brought into line. In most cases, orthodontic appliances, such as braces and retainers, will be used before and after the surgical phase of treatment, to ensure that you end up with an effective — and aesthetically pleasing — result.
Conditions that can be successfully treated with corrective orthognathic surgery include the following:
- Open bite, protruding jaw or receding chin
- Congenital defects such as a cleft palate
- Malocclusions (bite problems) resulting from underbites or severe overbites
- Obstructive Sleep Apnea, when more conservative methods fail
- Difficulty swallowing, chewing, or biting food
- Chronic jaw or jaw joint (TMJ) pain and headache
- Unbalanced facial appearance from the front or side
- Inability to make the lips meet without straining
- Chronic mouth breathing and dry mouth
- Facial trauma
The Surgical Procedure
While every patient’s needs are different, it’s possible to outline some typical steps in the process. The first (and perhaps most important) component is consultation and planning among members of the dental team, including the restorative or general dentist, the orthodontist, and the oral surgeon. Your overall plan may involve orthodontic treatments along with surgical procedures. Using diagnostic images, 3-D models and advanced software, a step-by-step plan will be developed for the entire process. It’s even possible in many cases to show you a picture of what you’ll look like when your treatment is finished.
The surgery itself may occur in a hospital or an office setting, with the type of anesthesia that’s most appropriate for the procedure, and for your comfort. Because the actual surgery is generally performed inside the mouth, it often leaves no visible traces. After the procedure, minor pain and swelling can be controlled by over-the-counter or prescription pain medication. A soft or liquid diet may be recommended for a period of time following the procedure.
Following surgery, your condition will be closely monitored — as will your progress through each phase of the treatment plan. When it’s complete, you can enjoy the benefits of improved functionality and an enhanced appearance.
Meet Your Top-Rated Family Dentist in Spokane Valley

Our Dental Services
Dental Crowns
Emergency Care
General Dentistry
Implant Dentistry
Orthodontics
Pediatric Dentistry
The Proof is in our Patients